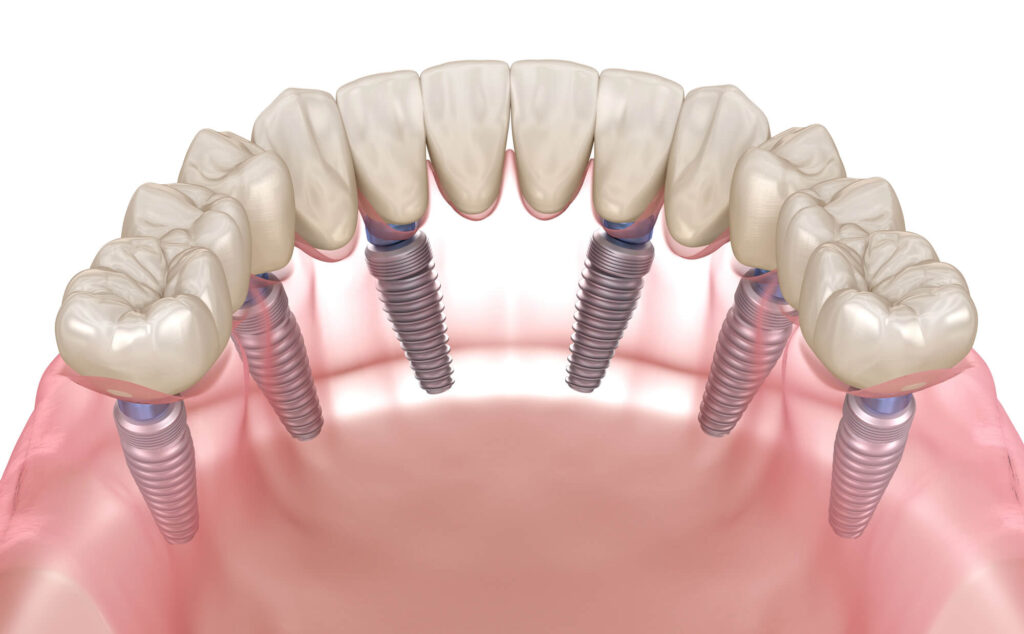
When you’re on the journey toward a full smile transformation with a dental implant procedure like the All-on-X or same-day implants, one essential part of the process is the temporary dental crown—often called a “healing set” at 4M Dental Implant Center. Think of it as a custom-designed, tooth-shaped cap that acts as a placeholder for your permanent dental crowns while your implants bond securely with your jawbone.
This transition period is more than just “waiting.” Your temporary custom dental crown plays a critical role in protecting the dental implant, maintaining bite alignment, preserving gum shape, and allowing you to smile with confidence during the healing phase. It’s a restoration that safeguards your investment while giving you the chance to get used to your new function, esthetics, and appearance before your permanent crown is placed.
Whether your temporary crown procedure involves a single implant, a dental bridge, or a full-mouth set, 4M’s approach is centered on precision, proper care, and your comfort. In this guide, we’ll explore the materials used for temporary sets, why 4M chooses zirconia for your finals, and how to care for your temporary crowns so you can move into your permanent smile with ease.
What Is a Temporary Dental Crown?
A temporary dental crown is a short-term restoration placed over your dental implant or natural tooth (in cases such as root canal treatment or dental bridges) to protect the site during healing. In implant dentistry, these temporary “caps” act as protective shields over titanium posts while osseointegration—the fusion of implant and bone—takes place. They are secured using dental cement or dental crown glue when used on natural teeth. For permanent crown placements on dental implants, a screw is used.
Why They’re Essential in the Transition Period
During this waiting period, temporary crowns serve several purposes:
- Protection: Safeguarding your implants from chewing forces and potential damage.
- Bite Alignment: Maintaining proper positioning of teeth and jaw to ensure a comfortable function later.
- Aesthetic Concerns: Preserving your smile and overall appearance so you feel confident in social and professional settings.
- Gum Health: Keeping gum tissue in shape for a seamless, permanent crown fit.
How 4M’s Temporary Crowns Differ
At 4M Dental Implant Center, our temporary crowns are custom-made from high-quality materials—all designed to balance appearance with the flexibility needed to act as a “safety buffer” for your new implants.
These crowns or caps are intentionally less strong than zirconia to protect the implant site; if something hard is bitten accidentally, the temporary crown may break first, sparing your implant from stress.
Nonetheless, that is not the ultimate purpose of the temporary crown, which is why all patients are urged to follow proper aftercare regimes and rules.
Common Materials for Temporary Dental Crowns
Contemporary dentistry and oral medicine rely on several temporary crown materials, although the following four are the most likely patients will encounter in quality dental implant centers.
Acrylic Resin
One of the most widely used options for a temporary dental crown is acrylic resin:
- Lightweight, easy to shape, and cost‑effective, making it ideal for the transition period after a dental implant procedure.
- Acrylic is often chosen for its smooth finish, which is gentle on surrounding gums, and its ability to be molded into a tooth-shaped “cap” and adjusted easily during follow‑up dental check‑ups.
- Less durable than permanent dental crowns, they are designed to be replaced once the healing process is complete.
Composite Resin
Composite resin is another common material in temporary crown procedures.
- Natural color and adaptable fit.
- Better appearance and aesthetics compared to some other temporary options.
- It can be bonded securely with dental crown glue or dental cement, and it provides moderate durability for chewing soft foods.
Composite resin crowns work well for patients needing a stable, attractive placeholder during the waiting period before receiving a permanent crown.
PMMA (Polymethyl Methacrylate) and Polyethyl Methacrylate
PMMA (Polymethyl Methacrylate), a high-polish plastic material, can also be frequently used for both single temporary crowns and full‑arch healing sets.
- Valued for its excellent appearance, high stain resistance, and the ability to mimic the look of a natural tooth.
- Polyethyl Methacrylate is a related option that offers similar properties but can be adjusted more easily during the placement and fitting process.
- Both materials are lightweight yet strong enough for daily function while protecting the implant or tooth underneath.
Metallic Materials
Although no longer necessary or used by most implant specialists, including 4M, in certain dental procedures, a metallic material was commonly used for a temporary crown.
- They were optimal when strength was critical.
- Useful in the back of the mouth, where chewing forces are stronger.
- However, due to appearance concerns, metallic options are typically replaced quickly with a permanent dental crown in ceramic or zirconia, or not used at all.
Patients should be aware of the advantages and differences between these materials to make the best and most informed decision possible, with the help of their dental healthcare provider.
Why These Materials Differ from Permanent Crowns
Temporary materials—whether acrylic, composite resin, PMMA, or metallic—are selected for their balance of function, cost, and removability.
Unlike zirconia or porcelain permanent crowns, these materials are not intended for decades of wear. Instead, they act as a safe placeholder, allowing for gum shaping, bite alignment assessment, and any necessary adjustments before the permanent crown is fabricated.

Temporary Crown Care and Maintenance Rules
During the weeks of healing period after a dental implant procedure, and after the first few days of taking medication and using cold compresses or ice packs to lower swelling, it’s essential to protect your temporary dental crown from unnecessary stress, contaminants, bad habits, and even protect yourself from enhanced sensitivity in teeth.
Follow a Soft Food Diet
- Stick to a soft food diet: Options like mashed potatoes, yogurt, scrambled eggs, and smoothies help reduce pressure on the crown and implant.
- Avoid sticky foods: But not too soft and chewy. Soft bagels, gum, chewy meat, and other sticky or chewy foods can grab hold of temporary crowns while chewing and dislodge them.
- Avoid hard or crunchy foods: This means nuts, hard candy, hard bread, and ice, which can cause damage, loosening, or even breakage.
This key rule in the temporary crown care guideline ensures that your restoration remains intact until your permanent crown is ready for placement.
Maintain Proper Dental Hygiene
Even though a temporary crown is a short‑term restoration, daily dental hygiene is still critical.
- Brush twice daily and gently around the crown using a soft‑bristled toothbrush. In natural teeth, pay attention to the gum line to prevent tooth decay. Special anti-sensitivity toothpaste might also be prescribed.
- Floss gently and carefully, preferably with a Waterpik or water flosser, as they will make cleaning the space around dental implants easier without causing movement or discomfort.
Be Mindful of Sensitivity and Discomfort
It’s common to experience mild sensitivity or pressure in the first few days after the temporary dental crown procedure. This can occur due to gum adaptation, bite alignment adjustments, or the temporary cement setting process. If you experience persistent discomfort, sharp pain, or swelling, contact your dentist promptly to address potential issues before they affect healing.
Schedule Regular Dental Check-Ups
Routine dental check‑ups during the waiting period allow your dentist to monitor implant stability, gum health, and crown fit. These visits are an opportunity to make any adjustments to bite alignment or shape before your permanent dental crowns are fabricated. Skipping check‑ups can lead to undetected potential challenges, such as loosening of the temporary crowns, decay at the crown margins in natural teeth, or complications with the implant site.
Avoid Harmful Lifestyle Habits
Certain habits can compromise both the temporary and permanent phases of your restoration:
- Smoking can slow healing and increase the risk of gum inflammation
- Excessive alcohol intake can affect bone health.
- Avoid using your teeth as tools, like opening packages or chewing non‑food items, as this can cause unexpected damage to the temporary crown.
Even with the best professional care and supervision, your dental implants’ long-term health will largely depend on how well you follow aftercare best practices.

Who Is a Candidate for Dental Implants with Temporary Crowns
A strong candidate for dental implants with a temporary dental crown typically meets the following criteria:
- Good overall health – No uncontrolled systemic conditions that could interfere with healing, such as unmanaged diabetes or severe cardiovascular issues.
- Healthy gums – Free from active gum disease, ensuring the implant site can support long‑term dental health.
- Adequate bone density – Sufficient jawbone structure to anchor the dental implant securely during the osseointegration process.
- Commitment to proper care – Willingness to follow all temporary crown care guidelines, including dietary adjustments, gentle flossing, and keeping up with an oral hygiene routine.
- Regular dental check‑ups – Understanding the importance of follow‑up visits to monitor healing, bite alignment, and crown stability during the transition period.
- Lifestyle habits that support healing – Avoidance of smoking or excessive alcohol consumption, both of which can slow recovery and increase the risk of implant failure.
Meeting these requirements helps ensure that the temporary crown serves as a reliable placeholder while protecting the implant site until the permanent dental crown can be placed.
Factors That May Require Additional Consideration
While many patients qualify for dental implants with a temporary dental crown, certain factors may present potential challenges and require additional planning or modification of the dental crown procedure:
- Medical conditions – Uncontrolled diabetes, autoimmune disorders, or other systemic issues may slow healing and increase the risk of implant complications.
- Lifestyle habits – Smoking, excessive alcohol use, or poor dental hygiene can reduce implant success rates and cause gum inflammation during the waiting period.
- Bite alignment issues – Problems with occlusion may put uneven pressure on the temporary crown, leading to discomfort, loosening, or premature damage.
- Bruxism (tooth grinding) – Chronic grinding or clenching can stress the restoration, so adjustments or protective appliances are necessary.
- Sensitivity and gum health concerns – Thin gum tissue or a history of gum recession may require additional care to ensure proper fit and esthetics of both the temporary and permanent crowns.
4M’s Comprehensive Evaluation Process
At 4M Dental Implant Center, candidacy is determined through a detailed assessment that includes dental impressions, 3D imaging, and a thorough examination of your bite, gums, and bone structure. This preparation allows us to customize both the temporary crown and the permanent restoration for optimal fit, function, and esthetics. The goal is to design a step‑by‑step procedure plan that ensures a smooth transition from your temporary crown to your long‑lasting permanent dental crowns.
What to Do if a Temporary Crown Breaks or Comes Loose
A temporary dental crown is designed to be a protective placeholder, but it’s not indestructible. Breakage or loosening can happen, especially if you bite into something too hard or experience unexpected pressure on the crown. Here’s how to handle the situation calmly and protect your dental health during the waiting period.
Immediate Steps to Take
- Stay calm: A broken or loose crown is rarely a dental emergency, but it should be addressed promptly to prevent damage to the underlying dental implant or natural tooth.
- Remove any loose fragments: Carefully take out any broken pieces to avoid swallowing or inhaling them.
- Rinse your mouth: Use warm water to gently rinse away debris and keep the area clean.
- Save the crown: Place the broken or loosened piece of acrylic, metal, ceramic, etc., in a small, clean container. Your dentist may be able to repair or recement it.
- Avoid chewing on that side: Prevent additional damage or discomfort by using the opposite side of your mouth until the restoration is fixed.
Temporary Solutions Until Your Appointment
If you can’t see your dentist immediately:
- Over‑the‑counter tooth repair kits: These can provide a temporary fix using a safe dental cement, but they are not a long‑term solution.
- Dental crown glue: Available in pharmacies, this can help hold the crown in place for a short time until your appointment.
- Soft diet: Stick to soft foods like soups, smoothies, or pasta to avoid putting pressure on the exposed area.
Why Prompt Repair Matters
- Protecting the implant site: An exposed dental implant post or prepared tooth is more vulnerable to damage, dental decay, infection, or gum irritation.
- Maintaining bite alignment: Leaving a missing or loose crown untreated can cause shifting in surrounding teeth and alter your bite.
- Preventing discomfort and sensitivity: Quick repair reduces the risk of gum soreness, tooth sensitivity, and complications with your final permanent crown placement.
At 4M Dental Implant Center, we can often replace or repair a damaged temporary crown quickly thanks to our in‑house dental lab and streamlined restoration process. This ensures your transition period stays on track and your final restoration is not delayed.

Why 4M Uses Zirconia for Permanent Crowns
While resins, composites, porcelains, and metals are best for temporary sets, there’s truly no better option in every aspect than zirconia and its characteristics for permanent teeth.
- Durability and Longevity: When it comes time to replace your temporary set of teeth with a permanent one, 4M Dental Implant Center chooses zirconia for its exceptional strength and endurance. Unlike acrylic or composite resin, zirconia is engineered to withstand years—often decades—of chewing forces without significant wear or damage. This high‑strength porcelain ceramic ensures that your restoration maintains its function and appearance long after the initial placement.
- Superior Aesthetics and Natural Appearance: Zirconia offers a life‑like translucency and shade‑matching capability that rivals natural enamel. This makes it ideal for patients who have both function and aesthetic concerns with regard to their smile. Zirconia permanent teeth are custom‑crafted to match the surrounding teeth in shape, color, and bite alignment, ensuring a seamless integration into your dental health and lifestyle.
- Biocompatibility and Gum Health: One of the major benefits of zirconia is its excellent biocompatibility. This means it’s kind to the gums, reducing the risk of inflammation or sensitivity that can sometimes occur with metallic materials. Over time, a zirconia permanent crown helps maintain healthy gum tissue around the implant site, supporting both the long‑term success of your dental implant and your overall dental hygiene.
- Resistance to Decay and Staining: Unlike some temporary crown materials that can discolor or wear down during the waiting period, zirconia is resistant to staining and does not promote dental decay around the margins. With proper care and maintenance, regular dental check‑ups, and consistent flossing habits, zirconia crowns retain their luster and keep your smile looking fresh for years.
Why Not Use Zirconia for Temporary Crowns?
While zirconia’s durability is unmatched, it’s not used for most temporary crown procedures for a key, and ironic, reason—flexibility.
Zirconia’s strength and durability create difficulties for the healing process and osseointegration period, when your teeth, gums, and bite may shift slightly. A temporary crown made from acrylic, PMMA, or composite resin allows for easier adjustments, removals, or replacements without risking the underlying dental implant. Once healing is complete, the zirconia permanent crown is placed as the final, long‑term restoration.
The Transition to Your Permanent Smile
Moving from a temporary dental crown to your permanent dental crowns is one of the most rewarding steps in your dental implant journey. This stage finalizes the restoration process, ensuring optimal function, esthetics, and long‑term dental health.
Healing Timeline
- Osseointegration period: Most patients spend several months in the waiting period, allowing the dental implant to fuse securely with the jawbone.
- Monitoring and adjustments: Regular dental check‑ups during this time help fine‑tune bite alignment, shape, and gum contour.
- Preparation for finals: Once the implant is stable, dental impressions are taken to fabricate your custom zirconia crowns.
Using the Transition Period to Your Advantage
- Testing fit and function: The temporary material lets you evaluate bite comfort, chewing efficiency, and speech clarity.
- Assessing esthetics: You can provide feedback on the appearance, including preference for tooth aspect, shape, and size, before the permanent crown is made.
- Identifying challenges: Any discomfort, loosening, or pressure points can be corrected before final placement, preventing long‑term issues.
Final Placement and Results
When the healing process is complete:
- Permanent crown placement: Your zirconia restoration is secured, providing a strong, durable, and natural‑looking finish.
- Function restored: You can return to a full diet, including firmer foods, without the limitations required during the healing period.
- Smile transformation: The final result is a stable, long‑lasting restoration that blends seamlessly with your natural teeth for optimal esthetics and confidence.
At 4M Dental Implant Center, this transition is a carefully managed process, ensuring your permanent crown placement is the perfect blend of precision, durability, and beauty.
From Healing Set to Forever Smile
Your temporary dental crown is more than just a placeholder—it protects your implant, maintains your bite, and shapes your gums for the perfect fit of your permanent crown. With proper care, quick attention to any issues, and 4M’s precision approach, the transition to your zirconia finals is smooth and rewarding.
Ready for your forever smile? Book your 4M Smile Assessment today and start the journey toward lasting confidence and function.