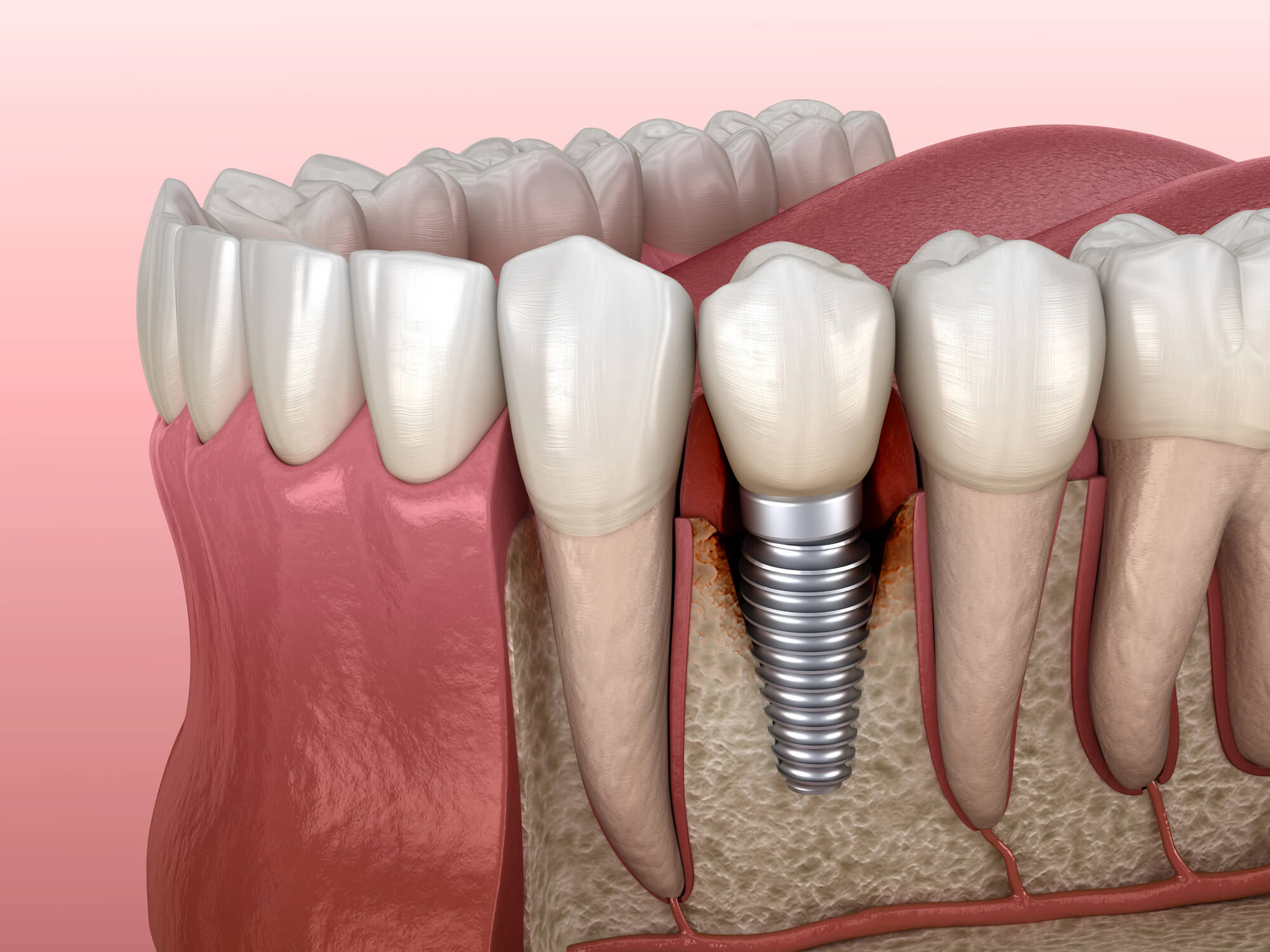
Modern dental implants are one of the most effective, durable, and natural-looking options for replacing missing teeth. Designed to mimic the structure of natural teeth, implants typically consist of a titanium screw or titanium alloy post embedded into the jawbone, topped with an abutment and crown. When placed properly and maintained through regular dental care, implant success rates exceed 95% and up to 99% at 4M.
But even with today’s advanced techniques, including digital dental implant diagnostics and guided bone regeneration, complications can still arise. For some patients, problems develop as early as during or shortly after dental implant surgery.
For others, symptoms emerge years later due to gum disease, chronic inflammation, or systemic health issues.
The good news? Most dental implant problems start with small warning signs that, if caught early, can be addressed before serious damage occurs. Whether it’s subtle discomfort, minor gum recession, or signs of infection at the implant site, knowing when to call your dentist could save your implant — and protect your long-term oral health.
The Difference Between Normal Healing and Warning Signs
Following dental implant surgery, it’s normal to experience some faint initial pain or soreness, mild swelling, and light bleeding for the first few days. This is your body’s immune system responding to the procedure and beginning the healing process. As the titanium post integrates with the healthy bone through osseointegration, the implant becomes stable, and symptoms should gradually subside.
Normal post-op healing may include:
- Mild discomfort for 3–5 days
- Swelling at the implant site
- Minor bruising or stiffness in the jaw
- Slight bleeding within the first 24–48 hours
However, not all symptoms should be brushed off as “normal.” Some signs may point to underlying implant complications, especially if they worsen over time or appear after initial healing.
If swelling worsens instead of improving, or if pain increases several days after surgery, it could be a sign of infection, rejection, or peri-implantitis.
Understanding the difference between standard post-op recovery and potential dental implant failure is critical for long-term success.
If something doesn’t feel right — or if symptoms appear unexpectedly — it’s always better to check in with your dental surgeon rather than wait.
7 Common Signs of Dental Implant Problems
While dental implants boast high success rates, problems can still arise, often starting subtly before escalating. Whether caused by infection, poor dental hygiene, or underlying medical conditions like diabetes or autoimmune disease, certain symptoms signal the need to contact your restorative dentist or dental surgeon right away.
Below are the most common and important signs to watch for if you suspect dental implant problems are developing.
1. Pain That Doesn’t Improve or Gets Worse
Some soreness is expected after implant surgery, but persistent or intensifying pain could indicate a deeper issue.
What to watch for:
- Throbbing or sharp pain several days or weeks after surgery
- Pain that increases rather than decreases over time
- Pain while chewing or touching the implant site
This may be a sign of infection, bone involvement, or failure in the bone regeneration process. The implant may be irritating nearby tissue or failing to fuse properly with the jaw bone.
2. Redness, Swelling, or Inflammation Around the Implant
Persistent swelling, puffiness, or redness of the gums around the dental implant may indicate early peri-implant inflammation or even peri-implantitis.
Key signs include:
- Swollen gum tissue near the implant
- Warmth or tenderness around the site
- Gum inflammation that doesn’t resolve with basic hygiene
These symptoms are often caused by bacterial buildup or poor plaque control, especially in patients with a history of gum disease or who smoke.
3. Bleeding Gums When Brushing or Flossing
Bleeding from the implant area isn’t normal and can indicate soft tissue irritation or infection.
Warning signs:
- Bleeding during routine brushing or flossing
- Bleeding triggered by light pressure or touch
- Metallic taste or slight discharge along the gumline
Unaddressed bleeding can lead to progressive gum damage or deeper infection that may compromise the implant.
4. Gum Recession or Visible Threads
Gum tissue should form a tight, healthy seal around the implant. If the gums begin to pull away, or if you see any exposed metal at the gumline, it’s time to call your dentist.
Indicators of gum recession:
- Visible threads or edges of the titanium implant
- The tooth appears longer or uneven
- Increased sensitivity along the gumline
Recession may result from inflammation, bone loss, or prosthetic misalignment and should be treated quickly to prevent deeper issues or dental implant failure.
5. The Implant Feels Loose or Moves
A dental implant should be as stable as a natural tooth. Even implant micro-movement is cause for immediate concern.
Signs of implant instability:
- Feeling like the tooth is shifting or wiggling
- Clicking or grinding sensations during chewing
- Perception of “give” when touching the implant with your tongue
This often signals failure of osseointegration, bone loss, or damage to the implant structure. Left untreated, the implant may fully detach from the jaw bone.
6. Pus, Bad Taste, or Foul Odor
Fluid discharge, unpleasant taste, or bad breath can all be signs of infection or peri-implantitis.
Watch for:
- White or yellowish pus from the gum or implant area
- Persistent bad taste, especially when chewing or swallowing
- Bad breath that persists despite good hygiene
These are often linked to bacterial infection or deep peri-implantitis lesions and require urgent treatment to prevent dental implant failure.
7. Difficulty Chewing or Bite Changes
If your bite feels “off” or if chewing becomes difficult after implant placement, the implant or crown may be out of alignment or the implant may be failing.
Symptoms include:
- Uneven pressure while biting
- Pain when chewing certain foods
- Teeth no longer fit together as they did before
This can be caused by improper loading of the implant, changes in the jawbone, or prosthetic issues, all of which should be evaluated during a dental consultation.
Schedule Your Free Consultation
Risk Factors That Increase the Likelihood of Dental Implant Problems
While dental implants are reliable and long-lasting, certain risk factors can significantly increase the chances of complications. Understanding your individual risk profile allows for better planning and proactive care.
Medical and Systemic Risk Factors
- Diabetes, especially when uncontrolled
- Osteoporosis or other bone metabolism conditions
- Autoimmune disease, such as rheumatoid arthritis or lupus
- History of immune suppression or certain medications (e.g., bisphosphonates)
- Genetic predisposition to gum disease or low bone density
These conditions may impair bone healing, reduce blood flow, or increase the body’s inflammatory response, making osseointegration more difficult and increasing the risk of implant rejection or failure.
Lifestyle Factors
- Smoking or vaping, which constricts blood vessels and impairs bone regeneration
- Poor oral hygiene and inconsistent plaque control
- Lack of regular dental checkups and professional maintenance
- Chronic bruxism (teeth grinding), which can damage implants or restorations
Patients who smoke are at significantly higher risk of peri-implantitis and long-term bone loss, making smoking cessation critical for long-term success.
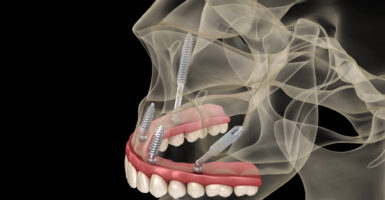
Surgical and Technical Factors
- Improper implant placement or angle during surgery
- Inadequate bone support or lack of pre-treatment bone grafts
- Use of poor-quality implant materials or components
- Failure to detect and treat early-stage gum disease before surgery
Choosing an experienced dental surgeon and completing necessary preparatory procedures like bone grafts or sinus cavity lifts can significantly reduce these risks.
When to Call Your Dentist
If you notice any changes in how your replacement teeth look, feel, or function, it’s always safer to reach out to your dental professional, even if the issue seems small.
Contact your dentist immediately if you experience:
- Pain or discomfort that gets worse after the initial recovery
- Visible gum changes, including recession, redness, or swelling
- Bleeding when brushing or flossing near the implant
- Difficulty chewing or an altered bite
- Signs of infection, such as pus or a persistent bad taste
- Any feeling that the implant is loose, mobile, or unstable
Don’t assume the issue will resolve on its own. Many implant problems can be corrected or reversed if caught early, especially when the dental team can intervene before the bone or soft tissues are significantly affected.
Even if you’re not sure whether a symptom is serious, your best option is to book a consultation with your implant dentist. A quick evaluation using digital imaging, clinical probing, and soft tissue assessment can provide peace of mind or identify problems before they escalate.
What Your Dentist Will Do
When you contact your dental office about potential implant problems, your care team will take a comprehensive, evidence-based approach to diagnosing the issue and preserving the implant if possible.
Initial Evaluation
- Visual inspection of the implant site and surrounding tissues
- Periodontal probing to assess pocket depth, bleeding, or inflammation
- Mobility check to determine if the implant abutment or root is loose
- Review of your medical history, medications, and risk factors
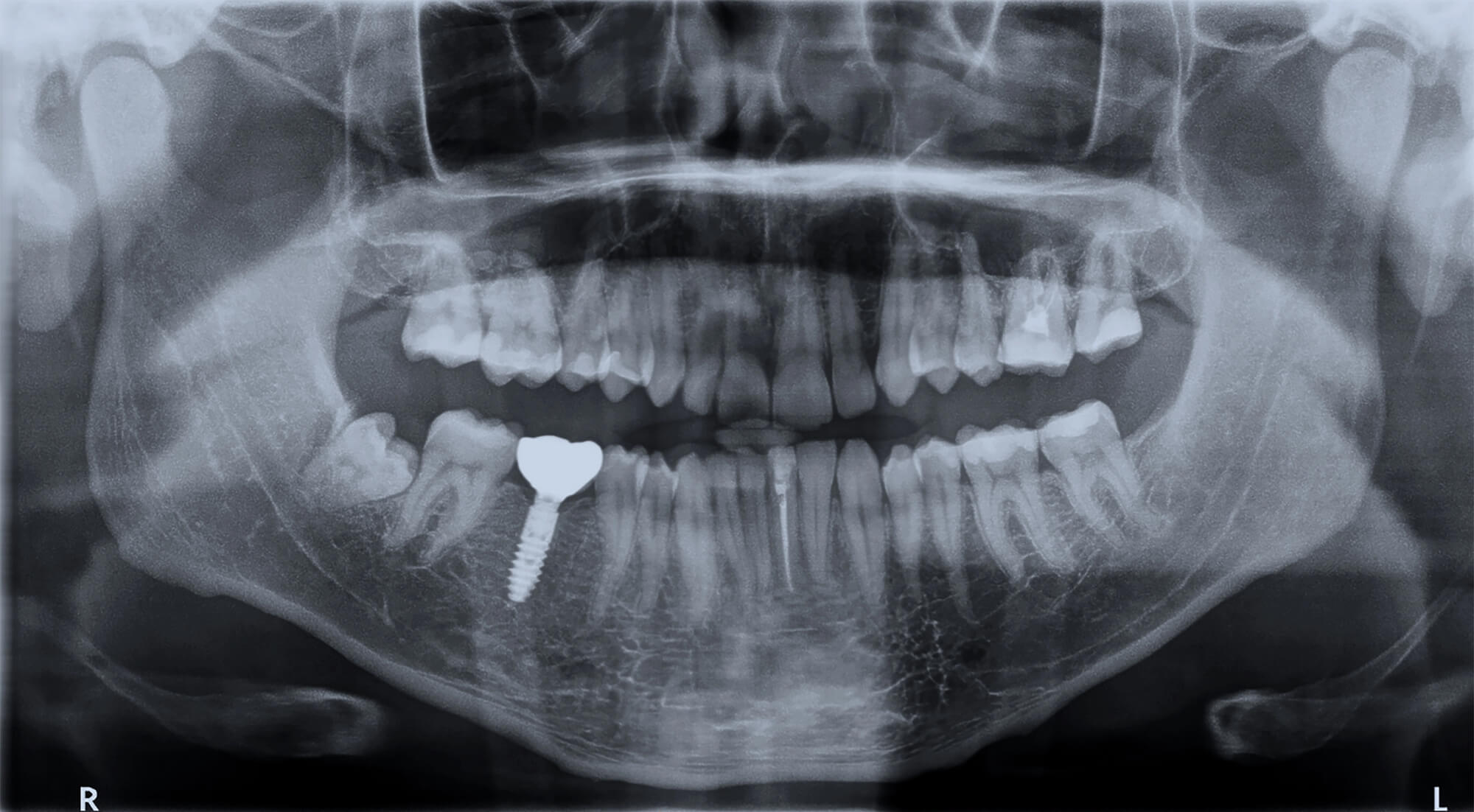
Diagnostic Imaging
- Intraoral radiographs (periapical or bitewing) to check for bone loss
- Digital imaging or CBCT scan to assess the implant’s position, surrounding bone, and integrity of osseointegration
These tools help your dentist identify whether the issue stems from soft tissue inflammation, peri-implantitis, mechanical complications, or more complex bone-related concerns.
Treatment Planning
Depending on the findings, your dental team may recommend:
- Professional cleaning and debridement of the implant site
- Local or systemic antibiotic therapy
- Adjustment or replacement of the implant abutment or crown
- Surgical intervention, such as guided bone regeneration or bone grafting
- In extreme cases of dental implant failure, implant removal and replacement
Prompt action can help avoid further complications, improve healing, and, in many cases, save the implant.
Preventing Future Implant Issues
The best way to avoid dental implant problems is to focus on prevention. A proactive approach before, during, and after dental implant surgery can significantly improve your chances of long-term success. Whether you’ve undergone a dental implant procedure recently or had dental implants for several years, maintaining excellent oral health is essential for avoiding implant failure and protecting the surrounding bone and gum tissue.
Maintain Excellent Oral Hygiene
Consistent oral hygiene is the foundation of implant dentistry and helps prevent gum disease and infection at the implant site.
-
Brush twice daily using a soft-bristle or electric toothbrush around the implant and your natural teeth.
-
Floss or use interdental brushes and water flossers to clean between the artificial tooth and adjacent teeth.
-
Use antimicrobial rinses as directed by your dental professional.
-
Attend regular dental cleanings and professional exams.
Good oral hygiene prevents plaque buildup and reduces the risk of peri-implantitis, bone loss, and other common dental implant problems. Keeping the tissues surrounding the implant healthy allows the titanium screw to remain stable as it fuses with the jaw bone during bone healing and new bone growth.
Schedule Regular Checkups
Regular dental checkups are critical for ensuring your dental implant procedure remains successful over time.
-
Visit your restorative dentist or oral surgeon every 3–6 months based on your individual risk factors.
-
Have radiographs or 3D scans taken annually to evaluate bone density and implant stability.
-
Make sure the crown, abutment, and replacement tooth remain properly aligned with the natural tooth root.
These visits allow your dentist to identify early warning signs such as swelling, loosening, or infection around the implant. Routine monitoring also ensures that any tissue damage, bone loss, or nerve or tissue damage is addressed before implant removal or implant failure becomes necessary.
Manage Systemic Health Conditions
Certain medical conditions can negatively affect the healing process and increase the risk of dental implant complications.
-
Keep diabetes and other medical conditions under control to promote sufficient bone healing and oral health.
-
Always update your dental team with your current medical history and medications.
-
Discuss concerns such as osteoporosis, low bone density, or autoimmune disorders with your oral surgeon before dental implantation.
Uncontrolled diabetes, autoimmune issues, and poor oral hygiene can interfere with bone grafting, bone growth, and the implant fuses process, reducing long-term success rates.
Avoid High-Risk Habits
Lifestyle choices play a huge role in the longevity of dental implants.
-
Quit smoking — it’s one of the top risk factors for implant failure and gum disease.
-
Address teeth grinding (bruxism) with a custom night guard to protect the implant site.
-
Avoid biting hard objects or using your teeth as tools, which can damage both the implant and your natural teeth.
-
Eat soft foods after implant surgery and during the healing process to prevent infection and minimize tissue damage.
Patients who smoke, grind their teeth, or apply excessive pressure around the implant are more likely to experience loosening, swelling, or persistent pain. These issues can compromise the surrounding bone and lead to an implant that lacks stability.
Your Body Sends Signals — Don’t Ignore Them
Dental implants are designed to replace missing teeth and restore full function, but they still require care and attention. If your body begins to show signs of discomfort, don’t dismiss them.
Pain or discomfort, perhaps a tingling sensation, swelling, or a loose implant can indicate infection at the implant, bone loss, or nerve damage. In severe cases, untreated infection may reach the sinus cavity or sinus cavities in the upper jaw, especially if the implant placement is close to these structures. Early detection and treatment by your dental professional are key to preventing serious complications or implant failure.
Protecting Your Investment
Dental implantation is a surgical procedure that involves precision, bone health, and commitment to maintenance. Every implant procedure — from initial bone graft to final restoration — depends on your oral hygiene and post-surgical care. Maintaining healthy gums, avoiding infection, and addressing potential complications promptly ensures your implant lasts as long as your natural tooth roots.
At 4M Dental Implant Center, our oral surgeons and restorative specialists use advanced imaging, careful implant placement, and long-term follow-up care to ensure each dental implant achieves optimal bone fusion and function. Whether you’re replacing missing teeth with immediate tooth replacement or managing existing dental implants, our goal is fewer doctor visits, improved overall oral health, and lasting confidence in your smile.
If you’re experiencing any signs of implant trouble, schedule a free consultation with 4M Dental Implant Center today.
Early action can save your implant — and your smile.






Reader Interactions