Dental implants have revolutionized the way we replace missing teeth, offering a permanent, stable solution through the use of titanium artificial roots that integrate with the jawbone. However, even the most successful dental implant treatment can face complications if oral hygiene is neglected or if certain risk factors are present.
One of the most serious and increasingly common complications in implant therapy is a condition known as peri-implantitis.
Peri-implantitis is a destructive inflammatory disease that affects the peri-implant mucosa (the soft tissues surrounding implants) and the supporting bone. It is typically preceded by a less severe inflammatory condition known as peri-implant mucositis that, if left untreated, can progress into severe peri-implant disease, leading to crestal bone loss, deep peri-implant pockets, and, ultimately, implant failure.
According to the American Academy of Periodontology and the American College of Prosthodontists, early diagnosis and consistent maintenance care are crucial for preserving the health of dental implants and preventing the irreversible damage associated with severe peri-implant disease.
In this guide, we’ll explore what causes peri-implantitis, how it can be prevented and treated, and what warning signs to watch for, whether you’re a new implant patient or have had your implants for years.
Understanding the Anatomy of the Problem
To understand peri-implantitis, it helps to first understand how dental implants work.
Dental Implants and the Surrounding Tissues
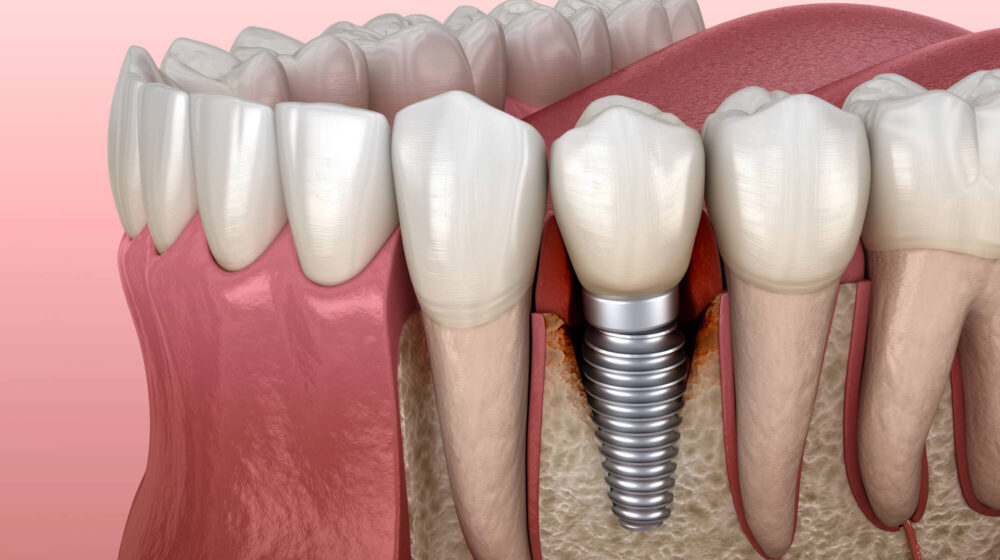
A typical implant is composed of three main components:
- A titanium implant (or titanium alloy screw) that acts as a replacement for the natural tooth root.
- An abutment that connects the implant to the visible restoration.
- A dental crown or bridge completes the tooth replacement.
Once surgically placed, the titanium artificial root fuses with the jawbone in a process called osseointegration, creating a strong, stable foundation. These osseointegrated endosseous implants restore both function and aesthetics, often lasting decades with proper care.
Surrounding this implant is the peri-implant tissue, including the peri-implant mucosa, which is similar to the gum tissue around natural teeth. Unlike natural teeth, however, implants lack periodontal ligament fibers, making them more vulnerable to microbial invasion and inflammation if plaque control is inadequate.
This soft tissue barrier must remain healthy and tightly sealed to prevent bacteria, plaque, and tartar from infiltrating the space around the implant and threatening the supporting bone.
What Happens During Peri-Implantitis?
Peri-implantitis is actually the more severe evolution of peri-implant mucositis, with both being the two main types of peri-implant diseases.
- Peri-implant mucositis: Peri-implantitis begins when bacterial plaque, specifically Gram-negative anaerobes and other periodontal pathogens, colonize the peri-implant sulcus, a fluid that accumulates around the implant. As biofilms mature and plaque accumulates, the host response triggers a gum inflammatory reaction in the soft tissues, or gum. This gum inflammation, called mucositis or peri-implant mucositis, does not immediately lead to bone loss.
- Peri-implantitis: However, if this inflammation spreads deeper into the peri-implant pocket, it can lead to progressive destruction of marginal bone levels.
Radiographic imaging, such as periapical radiographs or bitewing X-rays, often reveals bone loss before it becomes clinically visible. If left untreated, the damage becomes irreversible and may result in the loss of the implant entirely.
In fact, studies and systematic reviews have shown that once peri-implantitis lesions extend into the crestal bone, regeneration is challenging. That’s why early intervention during peri-implant mucositis is critical.
Common contributors to this bacterial cascade include:
- Lack of plaque control skills
- Infrequent dental check-ups
- Poor home and professional care strategies
- The presence of submucosal cement or poorly fitting prosthetics
Importantly, unlike gingivitis around natural teeth, inflammation around implants progresses more rapidly due to reduced vascularization and weaker defense mechanisms in peri-implant tissues.
Common Causes and Risk Factors
While peri-implantitis can affect any implant patient, certain behaviors, health conditions, and clinical factors dramatically increase its likelihood.
1. Poor Oral Hygiene and Plaque Buildup
The most common cause of peri-implant diseases is the buildup of bacterial plaque due to inadequate daily oral care. Biofilms rich in anaerobic bacteria begin forming within hours if left unchecked.
Key risks and mechanisms include:
- Colonization by gram-negative anaerobes and periodontal pathogens
- Inflammation of the peri-implant mucosa and destruction of peri-implant tissue
- Tartar buildup that exacerbates bacterial retention
- Accelerated crestal bone loss due to immune system overresponse
Patients with poor plaque control skills or inconsistent dental check-ups are most susceptible to this condition.
2. Peri-Implant Mucositis Left Untreated
Peri-implant mucositis is reversible; however, when left unattended, it often progresses into peri-implantitis.
Warning signs include:
- Red, swollen gums near the implant site
- Bleeding on brushing or during clinical peri-implant probing
- Transition from superficial inflammation to deeper bone involvement
Prompt professional intervention and at-home plaque control can prevent this escalation.
3. Smoking and Lifestyle Habits
Tobacco use negatively affects nearly every aspect of oral and systemic health, especially after implant placement.
Why smoking increases risk:
- Reduced blood flow to the oral tissues, impairing healing
- Weakened immune system, reducing infection defense
- Inhibited osseointegration during implant healing
- Increased rates of implant failure and bone loss
- Higher incidence of deep peri-implant pockets
Even light smoking can compromise the long-term success of implants.
4. Pre-Existing Gum Disease and Periodontal History
A prior history of periodontal disease, also known as gum disease, is a strong predictor of peri-implantitis. Periodontal disease is the inflammation and infection of the gums, which are the tissue supporting your teeth.
Poor oral hygiene is the most common cause of gum disease, and the infections associated with it can also lead to peri-implant diseases.
Contributing factors include:
- Persistence of periodontal pathogens in the oral microbiome
- Reduced host resistance in compromised tissues
- Transfer of bacteria to the peri-implant sulcus
- Incomplete healing or inflammation during implant therapy
- Undiagnosed residual pockets or inflammation near implant sites
Peri-patients must undergo complete periodontal treatment before implant placement.
5. Systemic Health Conditions
Medical conditions that compromise the immune response or impair healing increase susceptibility to peri-implantitis.
Common conditions include:
- Diabetes (especially uncontrolled)
- Autoimmune disorders like lupus or rheumatoid arthritis
- Conditions that impair collagen production or bone metabolism
- Reduced ability to combat bacterial plaque accumulation
Pre-surgical evaluation and interprofessional coordination are critical for these patients.
6. Surgical and Prosthetic Complications
Even the most skilled clinicians must adhere to strict protocol to avoid mechanical or technical causes of peri-implantitis.
Risk-enhancing factors include:
- Submucosal cement trapped under crowns
- Misaligned implants or poor angulation
- Excessive occlusal forces on prosthetics
- Loose abutments or misfitting prostheses
- Gaps where bacterial buildup can occur
Use of radiographic imaging, including periapical radiographs and 3D scans, helps catch these issues early.
Schedule Your Free Consultation

Warning Signs to Watch For
Peri-implantitis often begins silently, making early warning signs essential to recognize. If you’re a patient with one or more implants, staying alert to these symptoms can help prevent more serious damage.
Redness and Inflammation Around the Implant
Early inflammation is usually a sign of mucositis, not yet full-blown peri-implantitis — but it’s a critical warning stage.
Signs include:
- Red or swollen gums around the implant
- Sensitivity or tenderness when brushing
- Bleeding during tooth brushing or peri-implant probing
- Slight puffiness in the peri-implant mucosa
Pain, Discomfort, or Tenderness
Persistent discomfort is not normal once an implant has healed.
Look out for:
- Dull aching or pressure around the implant
- Pain when chewing or biting down
- Sensitivity when cleaning near the implant crown
Gum Recession or Implant Threads Becoming Visible
Soft tissue should fully cover the implant. If you can see part of the implant, there may be a problem.
Warning signs:
- Receding gum tissue
- Visible metal or threads near the gum line
- Elongated appearance of the implant crown
These are signs of soft tissue loss and/or bone resorption.
Persistent Bad Breath or Foul Taste
Bacterial imbalance can lead to odor and taste abnormalities.
Indicators include:
- Constant bad breath despite good hygiene
- Metallic or bitter taste
- Odor coming from the implant site
This may indicate a deep bacterial plaque reservoir.
Pus, Swelling, or Visible Drainage
These signs point to infection with possible bone loss.
Act immediately if you notice:
- White or yellow pus near the implant
- Swelling or painful nodules
- Spontaneous bleeding or discharge
Prompt treatment is needed to prevent implant failure.
Implant Mobility
An implant should be completely immobile. Any looseness is a red flag.
Watch for:
- Shifting or movement of the implant
- Clicking sensation when biting
- Pain when pressure is applied
Implant mobility often indicates advanced bone loss and disrupted osseointegration.

Diagnosing Peri-Implantitis
Early diagnosis of peri-implantitis is essential to prevent irreversible bone loss and preserve implant stability. Since the condition often starts without obvious symptoms, routine evaluations by a dental professional are critical.
Clinical Examination
During a dental check-up, the dental care provider will assess soft tissue health and look for early signs of inflammation via a peri-implant probing.
Evaluation typically includes:
- Visual inspection of the peri-implant mucosa for redness or swelling
- Bleeding on probing (a hallmark sign of peri-implant mucositis or peri-implantitis)
- Depth assessment of the peri-implant pocket using periodontal probing
- Detection of pus, mobility, or exposed implant threads
Probing depth of ≥6mm around an implant, especially with bleeding and suppuration, often signals peri-implantitis.
Radiographic Imaging
Radiographs play a crucial role in detecting crestal bone loss and monitoring marginal bone levels.
Common imaging tools:
- Periapical radiographs for the precise measurement of bone changes over time
- Bitewing X-rays to compare current bone levels to baseline post-placement scans
- Cone-beam CT (CBCT) scans in complex or unclear cases
A progressive reduction in marginal bone levels of 0.5mm or more per year after the first year of implant loading is typically considered pathological and may indicate peri-implantitis if accompanied by other clinical signs.
Risk Assessment
Diagnosis also involves evaluating risk factors to guide treatment urgency and customization.
Key considerations include:
- History of periodontitis or peri-implant disease
- Smoking habits
- Systemic conditions like diabetes or autoimmune disorders
- Level of plaque control and oral hygiene practices
- Time since implant placement and prosthetic loading
Integrating clinical, radiographic, and patient history helps ensure a diagnosis based on current guidelines, including the Classification of Periodontal and Peri-Implant Diseases and Conditions.
How to Treat Peri-Implantitis
Treatment for peri-implantitis depends on how advanced the disease is at diagnosis. While peri-implant mucositis can often be reversed with improved hygiene and professional cleanings, peri-implantitis usually requires a more aggressive, multi-layered approach.
Non-Surgical Treatment (Early Stage)
When caught early, non-invasive interventions may halt disease progression and allow tissues to heal.
Common non-surgical methods include:
- Professional mechanical debridement of the implant surface using non-metallic instruments
- Application of antiseptics such as chlorhexidine to reduce bacterial load
- Localized or systemic antibiotic therapy to suppress gram-negative anaerobes
- Use of ultrasonic devices or air abrasives to disrupt biofilms
- Improved patient education on plaque control and home care routines
Non-surgical therapy is most effective when the inflammation is limited to the peri-implant mucosa and no radiographic bone loss is present.
Surgical Intervention (Moderate to Advanced Stage)
Once peri-implantitis lesions extend into the supporting bone, surgical treatment is often necessary to regenerate tissue and remove infected material.
Surgical options may include:
- Flap surgery to access the implant surface for cleaning and decontamination
- Removal of granulation tissue and necrotic bone around the implant
- Bone grafting or the use of regenerative biomaterials to restore crestal bone levels
- Implantoplasty to smooth and reshape exposed titanium surfaces
- Laser treatments
- Removal and replacement of severely compromised implants
The choice of surgical technique depends on the defect morphology, implant system, patient health, and long-term prognosis.
Complementary Therapies and Maintenance
Long-term success requires sustained maintenance and post-treatment monitoring.
Critical aftercare strategies include:
- Ongoing dental check-ups and radiographic follow-up to monitor healing
- Reinforcement of personalized oral hygiene protocols
- Use of antimicrobial mouth rinses and irrigation devices
- Occlusal adjustments to minimize bite stress on the treated implant
- Maintenance of systemic health, including blood sugar control and smoking cessation
Once peri-implantitis has been managed, the patient enters a lifelong phase of implant maintenance, a critical period for preventing recurrence.
Schedule Your Free Consultation
Preventing Peri-Implantitis
While treatment options for peri-implantitis exist, prevention remains the most effective strategy. Fortunately, this condition is largely avoidable with the right combination of patient education, professional care, and daily habits.
Consistent and Effective Oral Hygiene
The foundation of prevention lies in removing bacterial plaque before it can mature into destructive biofilms.
Daily habits that reduce risk include:
- Gentle tooth brushing twice daily using a soft-bristled brush or electric toothbrush
- Daily flossing or use of interdental brushes around implants
- Incorporation of antimicrobial mouth rinses, such as chlorhexidine, under the guidance of a dental care provider
- Use of an air or water flosser to disrupt plaque in hard-to-reach areas
- Avoidance of aggressive brushing, which can damage the peri-implant mucosa
These home care strategies must be complemented by professional guidance to ensure proper technique and long-term consistency.
Regular Dental Check-Ups and Maintenance
Routine visits to your dental professional are essential to detect early signs of mucositis or monitor subtle bone level changes through radiographs.
Recommended frequency:
- Every 3 to 6 months for patients with implants, depending on individual risk
- Annual periapical or bitewing radiographs to track marginal bone levels
- Periodic periodontal probing to assess for bleeding, pocket depth, or mobility
Professional cleanings remove tartar and subgingival plaque that cannot be eliminated at home, significantly reducing peri-implant inflammation.
Risk Factor Management and Lifestyle Optimization
Patients can lower their risk of peri-implantitis by addressing systemic and behavioral risk factors.
Risk-lowering strategies include:
- Smoking cessation (even light smoking increases the risk of implant failure)
- Diabetes control, as poor glycemic regulation weakens the immune response
- Limiting alcohol intake, which may slow healing
- Managing autoimmune or inflammatory diseases in coordination with medical providers
- Avoiding mechanical trauma or excessive biting forces on implants
Preventing peri-implantitis is about total patient wellness and implant stewardship.

How 4M Dental Implant Center Prevents and Manages Peri-Implantitis
At 4M Dental Implant Center, peri-implantitis prevention is built into every phase of care, from consultation to long-term maintenance.
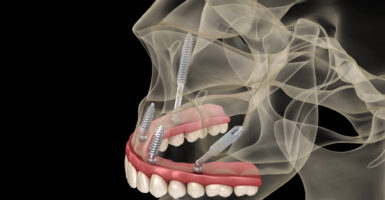
Precision-Guided Implant Placement
Successful implants begin with precision. Our implant surgeons utilize:
- Digital 3D imaging and CBCT scans for anatomical mapping
- Surgical planning protocols for exact implant positioning
- Selection of premium titanium implant systems with proven osseointegration success
- Careful soft tissue management to support healthy peri-implant tissue sealing
With expert placement and angulation, we reduce the risk of bacterial trapping and future inflammation.
Meticulous Prosthetic Fit and Cementation Protocols
Improper crown or bridge placement is a hidden but common contributor to peri-implant disease.
At 4M, we ensure:
- Use of custom abutments for ideal emergence profiles
- Elimination of submucosal cement, which can harbor bacteria
- Thorough checking of occlusion to minimize mechanical overload
- Use of zirconia crowns and bridges, which are smooth and resist plaque accumulation
Each prosthesis is designed to protect the implant and facilitate effective hygiene.
Individualized Hygiene and Maintenance Plans
Post-surgical care isn’t one-size-fits-all. Every 4M patient receives:
- A tailored hygiene plan based on risk assessment
- Instruction on brushing, flossing, and plaque control skills
- Antimicrobial rinse protocols during healing
- Take-home care kits, including a water flosser and oral health tools
- Lifetime access to check-ups and radiographic follow-up as part of our 4M Smile System packages
Our approach blends education, prevention, and proactive follow-through, ensuring implants remain stable, functional, and inflammation-free.
Long-Term Implant Health Starts with You
Peri-implantitis is a serious but preventable threat to your implant investment. It doesn’t happen overnight, but it is the result of silent inflammation, delayed intervention, and overlooked risk factors. Fortunately, patients who take an active role in their oral health can avoid it altogether.
Now that you know the causes, symptoms, and prevention strategies, you’re better equipped to protect your dental implants for life. And with the support of a comprehensive implant provider like 4M, you’re never on your own.
If you’re concerned about your implants or want to prevent peri-implantitis before it starts, schedule a free consultation with 4M Dental Implant Center today.
We’ll help you maintain a strong, stable, and inflammation-free smile for years to come.





Reader Interactions