Imagine a 55-year-old mom who, after years of struggling with unstable mini dental implants, walked into a 4M Dental Implant Center with fading confidence and a dental bridge that no longer fit. She’d invested time, money, and hope in a treatment that promised permanence but delivered constant discomfort, limited bite force, and daily embarrassment. Within weeks, she had a full-arch zirconia dental implant restoration designed specifically for her bone density and facial structure. Today, her smile is radiant, stable, and—most importantly—hers.
Her story isn’t unique.
Across the country, patients with failed or suboptimal implants are seeking a second chance at lasting oral health through dental implant revision surgery. Whether due to implant failure, outdated technology, or simply the natural evolution of your oral condition, the demand for minimally invasive implant revision is rapidly rising.
What Is Implant Revision?
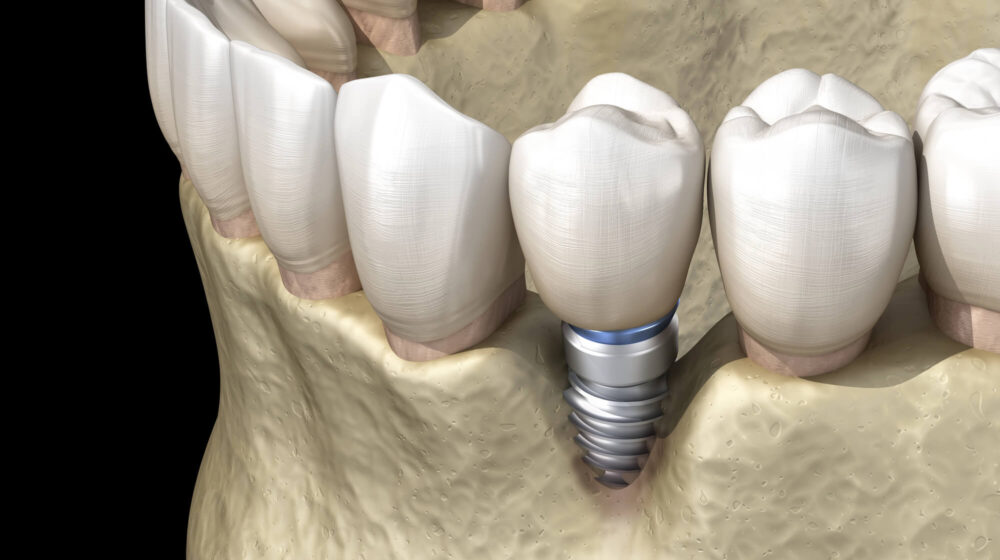
Implant revision is a specialized field of dental implantology focused on repairing, replacing, or upgrading previous implant treatments. It may involve correcting implant-supported crowns, addressing bone defects through guided bone regeneration, or replacing failing titanium posts or narrow-diameter implants with full-arch solutions like All-on-X.
Why “Minimally Invasive” Matters
Modern implant revision surgery has transformed from aggressive, multi-stage procedures into precise, digitally guided interventions. Using a wide range of techniques and tech like CBCT, 3D imaging, Hounsfield unit mapping, digital implant planning, and laser revisions (as preferred by 4M) many specialists in the industry can now:
- Minimize trauma to cortical bone and surrounding tissues
- Avoid extensive bone grafting or sinus lifts when possible
- Reduce healing time through custom smile design and same-day dental restoration
At 4M, we blend high-end evaluation technology, advanced materials like zirconia and biocompatible ceramics, laser revision techniques, and diagnostics to offer what few clinics can: predictable outcomes for even the most complex revisions.
Whether you’re living with implant-supported prostheses that no longer feel secure, or you’ve been told you’re not a candidate due to atrophic jaws, 4M’s minimally invasive revision options are designed to restore your smile, function, and self-confidence with clinical precision and human empathy.
Why Implant Revisions Are Sometimes Necessary
Implant revisions shouldn’t be viewed as only a fix for a broken smile. They can be an evolution toward what’s possible. Patients seek dental implant revision surgery not only due to failure, but often to upgrade materials, restore full function, or align their smile with who they’ve become.
Let’s explore the clinical, functional, and personal reasons why you might benefit from minimally invasive implant revision.
Clinical and Biological Causes
- Implant Failure or Mobility: When an implant loses its anchor in the jawbone due to poor osseointegration, infection, or overload, revision becomes necessary. These failures may be linked to improper torque values, undiagnosed bone quality issues, or improper surgical protocol, either with the bone grafts involved or the implants themselves.
- Peri-Implantitis: This inflammatory condition, similar to advanced periodontitis, can damage the surrounding soft tissue and cortical bone, leading to poor implant stability. It often arises from poor oral hygiene or ill-fitting prosthetic teeth and requires timely intervention to prevent broader oral health decline.
- Bone Loss or Resorption: If bone remodeling or grafting after implant placement is not managed correctly, especially in edentulous or frail patients, the supporting structure can deteriorate. This is particularly common with mini-implants or when CBCT imaging wasn’t used during initial placement.
- Poor Implant Placement or Angulation: Malpositioned implants may compromise occlusion, aesthetics, or even the stability of adjacent structures. Advanced revision cases may require guided surgery, ultrasound tools, or resonance frequency analysis devices to map implant stability before re-intervention.
- Suboptimal Materials or Mini-Implants: Patients who received mini or narrow-diameter implants, often without microcomputed tomography (micro-CT) or guided bone regeneration, are particularly at risk. These mini-implants often lack the biomechanical stability needed for full-arch support and can lead to discomfort, prosthetic failure, or reinfection.
Functional & Aesthetic Motivations
- Bite Adjustments: Even successful implants may require tweaking. If you experience discomfort, clicking, or occlusal imbalances, revision can improve chewing efficiency, jaw alignment, and long-term prosthetic function.
- Smile Confidence Boost: Your smile evolves with you. An implant-supported denture or ceramic crown placed a decade ago might feel bulky or outdated. Today’s prosthetic options—especially osseointegrated oral implants paired with zirconia bridges—offer a more natural look, seamless fit, and improved self-confidence.
- New Technology Access: Today’s dental prostheses are engineered with smart materials, and with digital imaging workflows. Whether it’s a zirconia restoration or revising mini-implants, current implant dentistry ensures that your revision reflects today’s best and tomorrow’s standards.
Warning Signs Your Implant Might Need Revision
If you’re experiencing any of the following, you may be a candidate for implant revision surgery:
- Persistent pain, swelling, or tenderness around the implant site
- Mobility or shifting of the implant post
- Receding gums or exposed implant threads
- Loose crowns or bridges
- Unpleasant odor, taste, or signs of infection
- Visible changes in bite, smile, or alignment
These symptoms may indicate issues like peri-implantitis, failed osseointegration, or prosthetic misalignment and require you to quickly book a dental professional, preferably a dental implant specialist.
With 3D CT scans, resonance testing, and a thorough review of your implant stability, 4M can accurately diagnose and guide your next step—without guesswork.

Key Facts About Minimally Invasive Implant Revision
Modern dental implantology has entered a new era—one defined by precision, efficiency, and minimally invasive techniques. If you’re facing the possibility of implant revision, it’s important to understand that today’s approach is drastically different from the invasive, multi-stage surgeries of the past
At 4M Dental Implant Center, dental restorations are guided by digital imaging, enhanced diagnostics, and biocompatible materials that protect your health, restore function, and minimize discomfort. Here’s what makes this approach so powerful.
What “Minimally Invasive” Really Means in Implantology
Minimally invasive doesn’t mean cutting corners—it means doing more with less trauma.
Rather than relying on wide incisions or exploratory methods, modern implant revision uses CBCT scans, 3D imaging, and guided implant placement to limit disruption of the surrounding jawbone, soft tissue, and existing implants. Here’s how:
- Preservation of surrounding bone and soft tissue: Bone grafting, sinus lifts, and ridge augmentation are sometimes avoidable using advanced digital implant planning and growth factor-assisted healing, especially when the cortical bone and surrounding structures are intact.
- Smaller incisions and less trauma: With digital implant guides, our implant specialists create just enough access to perform precise work—protecting vascular supply and encouraging faster healing through improved bone ingrowth.
- Guided implant surgery using CBCT and digital scans: Every revision is mapped using cone-beam computed tomography. We analyze bone density, plan insertion angles, and ensure optimal implant stability, all before the first incision is made.
- Faster recovery and reduced downtime: Patients experience significantly less swelling, pain, and downtime compared to traditional surgeries. Many walk out with same-day dental prostheses or custom temporary restorations—smiling confidently just hours after treatment.
This minimally invasive philosophy for all dental restorations is particularly important for patients with atrophic jaws, edentulism, or previous implant failure from poorly placed mini dental implants. It not only shortens recovery time but also improves long-term outcomes by preserving the biological environment essential for osseointegration.
4M’s High-Tech Approach to Implant-Supported Restorations
At 4M, we leverage every layer of innovation to offer best-in-class outcomes for even the most complex revision cases, which has helped us maintain our 99.9% success rate.
- CBCT and 3D Digital Imaging for Diagnostics: We use CBCT scans and micro-CT analysis to evaluate bone defects, map nerve proximity, and assess previous implant placement. This allows us to avoid unnecessary trauma and select the ideal implant site with precision.
- In-House CAD/CAM Lab and Digital Implant Design: Our integrated CAD/CAM lab enables real-time collaboration between surgeons and lab technicians. This means custom smile design, same-day prosthetic teeth, and immediate adjustments based on intraoral feedback.
- Zirconia and Biocompatible Ceramic Restorations: Unlike many legacy restorations that use metal or outdated polymers, we prioritize zirconia and ceramic prosthetic options for strength, aesthetics, and long-term biocompatibility. These materials reduce plaque accumulation, enhance gum health, and look indistinguishable from natural teeth.
- PRP and PRF Healing: We apply PRP (Platelet-Rich Plasma) and PRF (Platelet-Rich Fibrin) in dental implants to enhance healing and bone regeneration after implants or bone grafts.
- Osseointegration Monitoring: After revision, we monitor healing and offer real-time insight into implant stability without invasive probing.
- Customized Aftercare & Hygiene Protocols: Every 4M patient receives a tailored maintenance program, including guidance on oral hygiene, bite force management, and tools to preserve the longevity of their implant-supported restoration.
This synergy of technology, expertise, and personalization is what makes our minimally invasive implant revision approach not just possible—but life-changing. It ensures that your next implant isn’t just better but built to last.
Schedule Your Free Consultation
4M’s Preferred Full-Mouth Solutions: All-on-X & Same-Day Dental Implants
For patients needing implant revision—especially those dealing with failing mini dental implants, loose dentures, or chronic bite issues—4M’s signature solutions offer a new beginning. Our full-arch options, including the All-on-X system and same-day dental implants, are engineered for long-term success, even in complex cases with limited bone or previous prosthetic failure.
These treatments aren’t one-size-fits-all. They’re precision-built using digital diagnostics, advanced materials, and real-time implant planning—all designed to get you smiling again with stability, confidence, and comfort.
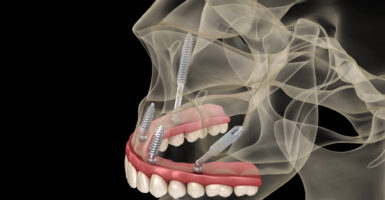
What Is All-on-X? Why It Works for Revisions
The All-on-X system is a revolutionary approach to full-arch restoration. Instead of replacing each missing tooth with a separate implant, this system uses four to six strategically placed implants—often tilted to maximize use of available jawbone—to support a full-arch fixed prosthesis.
This method is particularly effective for patients with:
- Failing narrow diameter implants or mini-implants
- Severe bone loss in the posterior maxilla
- Unstable overdentures or incomplete restoration
- Edentulism caused by dental diseases, periodontitis, or trauma
Why it excels in revision cases:
- Avoids bone grafting in most cases: Thanks to angled placement and the use of dense anterior bone, All-on-X can often eliminate the need for extensive bone grafting, sinus floor elevation, or ridge augmentation.
- Reduces load on compromised bone: The design distributes bite force efficiently across the arch, improving overall implant stability and reducing the risk of overload, which is common in revisions.
- High success rates: Clinical trials and our own years of experience have shown high long-term, 99.9% success rates for All-on-X systems, especially when combined with digital imaging, CBCT-guided planning, and materials like zirconia.
- Restores full function and aesthetics: Patients report stronger bite force, better occlusion, and higher satisfaction compared to single implant revisions or denture-based systems.
All-on-X is ideal for patients with a history of implant failure, peri-implantitis, or unsatisfactory results with removable prosthetic options.
Same-Day Smile Options for Revision Cases
Time matters—especially when you’re living with the discomfort or embarrassment of a failing implant. At 4M, we’ve refined the art of same-day full-arch treatment so you can arrive in the morning with a problem and leave in the afternoon with a solution.
Here’s how the process works:
- Digital implant planning with CBCT and CT scans: We map your anatomy in 3D to identify optimal implant placement sites based on bone density, jaw contours, and previous implant positions. Planning includes evaluating cortical bone thickness to ensure maximum primary implant support.
- Immediate implant placement and temporary prosthetic delivery: Titanium posts are placed precisely using guided surgery, followed by delivery of a custom-designed temporary prosthesis. This avoids the need for extended healing with an open site or ill-fitting denture.
- In-house fabrication of prosthetic teeth: Using CAD/CAM technology and our on-site lab, we produce high-quality, aesthetic provisional restorations in real time—without outsourcing or delays.
- IV sedation and local anesthesia: Revision cases are often emotionally and physically taxing. We offer full sedation options to make the experience as smooth and pain-free as possible, especially when removing mini implants or correcting previous surgical trauma.
- Final zirconia or ceramic prosthesis delivery after healing: Once osseointegration is confirmed, we deliver your final implant-supported prosthesis using durable materials that are biocompatible, stain-resistant, and precisely contoured for natural occlusion.
For patients suffering from atrophic jaws, loose dentures, implant instability, or prosthetic wear, same-day solutions offer a fast track to restoration, with no compromise in quality or safety.
Whether it’s All-on-X, immediate full-arch treatment, or custom protocols tailored to your anatomy and oral condition, 4M’s solutions redefine what’s possible in implant revision dentistry.

Types of Implant Revisions: From Simple Fixes to Full Redos
Implant revision is not a one-size-fits-all process. Some patients need minor adjustments, while others require full reconstruction of failed or outdated work to achieve implant stability. At 4M Dental Implant Center, we offer a spectrum of implant revision surgery options, tailored to the severity of the issue, the health of your bone and gums, and your personal goals.
From repairing a loose crown to reengineering full-arch implant-supported restorations, our implant dentistry team uses advanced diagnostics like CBCT, digital imaging, and microcomputed tomography to determine the most effective path forward.
Here’s a breakdown of the most common types of dental implant revision procedures.
Crown or Abutment Replacement
Sometimes, the implant itself is healthy and fully integrated into the jawbone, but the prosthetic teeth above it—the crown or bridge—have worn out, loosened, or become damaged.
Indications for this revision:
- Chipped or cracked ceramic crowns
- Loose abutments causing discomfort or bite changes
- Poor aesthetic match or outdated color and shape
- Inadequate occlusion or poor bite force distribution
These cases of damaged or improperly fitted crowns are generally treated without disturbing the implant post and require no invasive surgical approach. We assess implant stability to confirm the post is still osseointegrated and whether there’s a need or not for a bone graft before designing a new crown or bridge using advanced ceramic or zirconia materials.
Implant Removal & Replacement
If the implant post itself has failed—due to infection, misplacement, or loss of integration—it may need to be removed and replaced.
Common causes:
- Peri-implantitis
- Osseointegration failure
- Pain or swelling at the implant site
- Posts placed without proper bone assessment or digital planning
- Insertion into compromised cortical bone or atrophic jaws
At 4M, implant removal is done using minimally invasive surgical approaches, often under IV sedation and local anesthesia. After removal, we use digital tools to assess bone density and anatomical landmarks before re-inserting a new implant—typically a more robust titanium post with guided support and improved angulation.
When needed, bone grafting or guided bone regeneration techniques using growth factors are performed to restore the implant site.
Full Mouth Reconstruction
Patients who received mini dental implants, had outdated or piecemeal work from multiple providers, or wore failing overdentures for years often require a comprehensive revision.
These cases may include:
- Multiple failing implants or prostheses
- Severe bite misalignment or jaw instability
- Thin ridge anatomy from long-term edentulism
- Prior systems that lacked proper implant design due to a lack of digital planning or material integrity
Our full-mouth revision strategy includes:
- CBCT-driven digital planning and 3D imaging
- Removal of all failing components
- Placement of new implant-supported restoration using All-on-X or custom configurations
- Fabrication of interim and final dental prostheses in-house
- Close monitoring of osseointegration, healing, and soft tissue adaptation
This approach transforms function, aesthetics, and long-term oral health, while protecting against future implant complications.
Additional Surgical Procedures (If Needed)
In complex revision cases, supportive procedures may be required to rebuild the structural foundation needed for implant success:
- Osteotomy: Minor reshaping of the bone to improve implant insertion angles and stabilize the base.
- Sinus Lift: Elevating the sinus floor and augmenting the area with bone material to enable posterior maxilla implant placement.
- Bone Grafting: Replenishing lost bone due to trauma, resorption, or long-standing edentulism. We utilize smart materials, autografts, and biocompatible membranes to promote healthy bone ingrowth.
These procedures are often performed during the same appointment as implant removal or insertion, depending on bone quality and patient health. At 4M, we prioritize minimally invasive protocols that reduce trauma and speed up healing.
Materials Matter: Why Suboptimal Implants Often Fail
The materials used in your original implant procedure have a direct impact on long-term success—and in many revision cases, they are a root cause of failure. From mini dental implants with low load-bearing capability to outdated metals with poor biocompatibility, material choice often determines whether an implant will integrate, function, and last.
At 4M Dental Implant Center, we frequently see revision cases involving mini-implants, also known as narrow-diameter implants, and non-guided placement, or restorations fabricated without the benefit of digital imaging or CBCT planning. Let’s explore why material matters—and why 4M uses only proven, patient-safe options.
The Problem with Mini-Implants
While mini dental implants may seem appealing due to their smaller size and lower upfront cost, they often fall short in full-arch or high-force areas. Originally designed for temporary stabilization or narrow ridges, they are now frequently misapplied in complex cases without proper planning or long-term consideration.
Why mini-implants often lead to revision:
- Insufficient support for full-arch prostheses: Their smaller diameter reduces contact with the jawbone, limiting osseointegration and making them vulnerable to micromovement and failure.
- Poor load distribution: Because they lack the mechanical strength of standard titanium posts, mini-implants tend to overload adjacent bone and surrounding structures, increasing the risk of bone defects and resorption.
- Placement without guided imaging: Many mini-implant procedures are performed without digital implant planning or even 3D CT scans, leading to suboptimal placement angles and reduced implant stability.
- Higher rates of peri-implantitis: Due to their reduced width and surface area, mini-implants are more prone to inflammation and peri-implantitis, especially if oral hygiene or occlusion is not well maintained.
Patients who received mini-implants years ago often return with failing implant-supported restorations, discomfort, or fractured posts—making them prime candidates for implant revision surgery with more durable materials.
Why Zirconia and Titanium Dominate at 4M
At 4M, we only use materials supported by clinical trials, biocompatibility data, and long-term performance metrics. Whether you’re receiving a new implant or replacing a failing one, material integrity is non-negotiable.
Zirconia Bridges and Restorations
- Metal-free and aesthetic: Zirconia provides a bright, natural appearance ideal for full-arch dental prostheses and visible zones. It resists staining and is highly durable, even in patients with high bite force or parafunction.
- Biocompatible and plaque-resistant: Zirconia does not corrode or promote bacterial buildup, reducing the risk of inflammation, peri-implantitis, or adjacent gum recession.
- Ideal for patients with allergies or sensitivity: For those sensitive to metals or seeking a more holistic approach, zirconia provides a safe, long-lasting alternative.
Titanium Posts
- Gold standard for osseointegration: Titanium has been used for decades due to its high strength-to-weight ratio, corrosion resistance, and proven osseointegration properties. It forms a stable, direct bond with bone, supporting long-term stability in single and full-arch applications.
- Versatile across bone types: Whether your jawbone has reduced volume, irregular ridges, or variable bone density, titanium implants can be placed using angled techniques and guided bone regeneration to support even challenging cases.
- Supports full digital workflows: Titanium posts integrate seamlessly with CAD/CAM abutments and prosthetics, ensuring precision fit, proper occlusion, and reduced chair time during revisions.
4M’s success rate has depended on removing all outdated materials from our process and rebuilding with precision-designed zirconia prosthetic teeth or titanium implants. Patients gain more than just strength—they gain peace of mind, restored confidence, and a smile that’s built to last.

Diagnostic Excellence: How We Plan the Ideal Revision
Every successful implant revision begins with one essential step: a precise, evidence-based diagnosis. At 4M Dental Implant Center, we treat revision cases with the same rigor as complex surgeries—because they are. Whether we’re removing failing mini dental implants or planning a full-arch restoration, our 99.9% success rate protocol leaves nothing to guesswork.
Using advanced technologies like CBCT, photogrammetry, and dental lasers, we assess not just your symptoms, but the entire biological, structural, and prosthetic ecosystem influencing your outcome.
Digital Smile Design & CBCT Imaging
The foundation of revision success is a deep, accurate understanding of what went wrong—and what can be done better.
- CBCT (Cone-Beam Computed Tomography)
Unlike traditional X-rays, CBCT provides 3D imaging of your full maxillofacial structure. We analyze bone density, implant angulation, proximity to anatomical landmarks, and the condition of surrounding structures. - Digital Smile Design (DSD)
We use DSD to plan not just the placement, but the aesthetics of your smile. This allows us to align your restoration with facial proportions, lip dynamics, and functional occlusion for long-term stability and natural appearance. - CT scans and intraoral digital imaging
These tools offer enhanced visualization of prosthetic fit, bone remodeling, and even early signs of peri-implantitis, enabling preventative intervention before complications escalate.
Bone Density & Quality Assessments
Understanding the condition of your bone is central to successful implant revision—especially if you’ve had implants placed without proper evaluation or have experienced long-term edentulism or bone defects.
Our team assesses:
- Bone quality: Using CBCT and CT-derived data, we identify dense vs. porous regions in both cortical and trabecular bone.
- Bone volume: Measuring ridge width and height to ensure sufficient support for new implant posts.
- Bone remodeling status: Identifying whether your jawbone has undergone resorption due to missing teeth, pressure from ill-fitting dentures, or previous implant trauma.
If deficiencies exist, we may recommend guided bone regeneration, sinus lift, or the use of growth factors to enhance bone ingrowth prior to re-implantation.
Precision Execution with Guided Surgery
Once the diagnostics are complete, we translate data into precision:
- Digital implant planning software: Allows us to pre-plan each implant’s depth, angle, and position in relation to nerves, sinus structures, and adjacent prosthetics.
- Custom surgical guides: Printed in our lab and used during surgery to ensure exact placement with minimal deviation—protecting surrounding bone and tissues.
The result? A more accurate, less invasive procedure with higher implant success rates, reduced healing times, and longer-lasting outcomes.
Schedule Your Free Consultation
Benefits of Minimally Invasive Implant Revision
When your current implants aren’t working—or weren’t done right the first time—choosing the right path forward can feel overwhelming. But minimally invasive implant revision offers more than just a technical fix. At 4M, it’s a carefully designed process to restore comfort, function, aesthetics, and confidence without the stress of traditional surgical procedures.
Less Trauma and Downtime
- Smaller incisions and soft tissue preservation mean minimal disruption to your existing anatomy.
- Avoidance of extensive bone grafting or sinus lift procedures whenever possible.
- Precision-guided tools and digital planning reduce the need for exploratory surgery.
- Patients typically experience less swelling, reduced bleeding, and a faster return to normal activity.
This is especially beneficial for older patients, those with frailty or sarcopenia, or individuals concerned about surgical recovery time.
Lower Complication Rates
- Advanced diagnostics like CBCT and 3D imaging help avoid critical structures and reduce surgical risks.
- Use of biocompatible materials like zirconia and titanium heightens the success rate and protects against adverse reactions or prosthetic incompatibility.
- Digital planning ensures ideal occlusion and bite force distribution, preventing overload on new implants.
All these factors contribute to a more stable result with fewer post-operative concerns and less likelihood of a secondary revision.
High Patient Satisfaction
- Our custom smile design process ensures that aesthetics are matched to your face, personality, and lifestyle—not just to a mold.
- We use state-of-the-art lab technology to produce implant-supported restorations that feel and function like natural teeth.
- Many patients report dramatic improvements in eating, speaking, and smiling just days after their revision.
Our dental professionals have helped thousands of patients upgrade from failing overdentures, poorly placed narrow-diameter implants, or mismatched prosthetics to smiles that are natural-looking, secure, and built to last.
Immediate Functional and Aesthetic Results
- With same-day smile options, patients often receive new provisional teeth on the day of surgery.
- You leave with a smile you’re proud to show—not a gap, a temporary denture, or a long wait for results.
- Final zirconia or ceramic prosthetic options are delivered after healing, offering unmatched durability and beauty.
This immediate impact supports emotional healing alongside physical restoration—especially for patients who’ve struggled with failed implants or long-term edentulism.
Long-Term Oral Health Stability
- Revisions that address underlying causes—such as peri-implantitis, improper angulation, or bone loss—prevent future issues.
- With proper placement, material selection, and maintenance, revised implants can last for decades.
- We educate each patient on oral hygiene, implant care, and how to maintain stability through follow-up evaluations and cleanings.
In short, minimally invasive doesn’t mean minimal impact. It means achieving maximum results with minimal disruption—and that’s exactly what we deliver.

Why Choose 4M for Your Implant Revision
If you’ve been told you’re not a candidate for implant revision… think again.
At 4M Dental Implant Center, we specialize in solving cases that others turn away. Whether you’re dealing with failed mini dental implants, fractured posts, a loose overdenture, or previous implant work that just doesn’t feel right, our full-spectrum revision protocol is built around one thing: your success.
Here’s why thousands of patients trust 4M to restore their health, their function, and their smile.
- A 99.9% Candidacy Rate: We’ve developed protocols that allow us to treat nearly all revision cases—even those involving severe bone loss, atrophic jaws, or systemic concerns. Custom revision paths are mapped based on bone quality, occlusion, and implant history. In cases of prior rejection, 4M often provides second opinions that lead to successful outcomes. By combining digital imaging with advanced surgical techniques and strategic implant positioning, we make dental implants accessible to more patients than ever.
- Same-Day Smile Options: Where many clinics require multiple months of healing before delivering results, we accelerate the process using digital planning and in-house fabrication. This protocol shortens recovery time and reduces the emotional toll of long waiting periods.
- Lifetime Warranty on Implant Restorations: We believe your investment should last. That’s why we offer a lifetime warranty on implant-supported restorations—paired with a personalized oral hygiene and aftercare plan to keep your new smile functioning beautifully for decades.
- In-House Team, Technology, and Care Continuity: From your first consultation to your final set of teeth, everything happens under one roof, thanks to our team of full-time dental implant surgeons and designers on staff. No referrals. No third-party delays. Just direct, comprehensive care from a team that understands your full implant story.
- Expertise in Full-Arch and Revision Dentistry: We aren’t just placing implants—we’re solving problems. Our team is specially trained in revision strategies for complex cases involving: Narrow diameter implants; Bone grafting and guided bone regeneration; Misaligned or failed implant placements; Non-biocompatible materials and prosthetic mismatches; Bite force misdistribution and occlusal issues
At 4M, you’re not just fixing a failed implant—you’re entering into a higher standard of care.
Who Is a Good Candidate for Revision
Not all implant failures are dramatic. Sometimes it’s a subtle shift in your bite. Other times, it’s discomfort that never fully goes away. And in many cases, patients simply know something isn’t right—but haven’t been given a clear answer.
At 4M Dental Implant Center, we take a holistic approach to determining candidacy for implant revision. If your implants were placed years ago, if you received mini dental implants with disappointing results, or if you’re unhappy with your smile’s look or feel, you may be an ideal candidate for minimally invasive implant revision.
Here are some of the most common situations we treat:
Mini-Implant Failure Cases
If you’ve received mini dental implants and are now experiencing mobility, pain, gum recession, or functional limitations, revision may be necessary. These narrow-diameter implants are not ideal for full-arch support or patients with moderate to high bite force, and they often require removal and replacement with more stable, osseointegrated prostheses.
You may be a candidate if you experience:
- Looseness or movement of implants
- Visible threads or receding gum tissue
- Difficulty chewing or poor denture support
- Chronic inflammation or signs of peri-implantitis
Patients with Failed Single Implants or Bridges
Sometimes, a single implant or bridge that initially seemed fine starts to fail due to poor angulation, occlusal stress, or biologic complications like bone loss or soft tissue decline. If left untreated, the surrounding bone may become compromised, reducing future implant success.
Revision may involve:
- Removing the original post
- Correcting bone or tissue defects
- Replacing with a new implant and crown, planned using digital imaging
Loose Dentures or Hybrid Prosthetics
Patients with denture-based or bar-supported prosthetics often come to us after years of dealing with poor retention, instability, and discomfort. These cases typically benefit from transitioning to fixed implant-supported restorations using the All-on-X system or same-day protocols.
Candidates in this group often:
- Have been wearing removable overdentures for years
- Experience poor fit, clicking, or movement during speech or eating
- Want to eliminate adhesives or plate coverage on the roof of the mouth
- Need improved self-confidence and long-term comfort
Edentulous Patients Ready to Upgrade
Even if you’ve been living with full edentulism—no teeth at all—you may still have the bone, health, or resources to pursue a more permanent solution. Revision doesn’t always mean correcting past implants; it can mean correcting past decisions or limitations.
Ideal candidates:
- Have adequate bone for implant placement or are open to guided bone regeneration
- Seek a permanent solution to replace dentures
- Want restored chewing function, bite force, and facial structure
- Are committed to maintaining their oral hygiene and follow-up care
Cases Previously Denied by Other Clinics
Perhaps you were told you didn’t have enough bone. Or maybe another provider wasn’t equipped to remove failed implants or design a full-arch restoration. At 4M, we specialize in the complex, the turned-away, and the “impossible.”
Using CBCT imaging, digital workflows, and expert surgical planning, we’ve helped patients who were:
- Rejected due to atrophic jaws or systemic conditions
- Turned down because of past implant failures
- Misdiagnosed with unfixable bite issues or occlusion problems
Our goal is simple: to say yes where others said no—safely, effectively, and with long-term success.
FAQs About Implant Revision & Recovery
How long does implant revision take?
The duration depends on the complexity of your case. Minor revisions like crown replacement may take one visit. More complex cases involving implant removal, bone grafting, or full-arch reconstruction can span several months. However, many patients receive temporary prosthetic teeth on the same day using 4M’s immediate restoration protocols.
Will I be without teeth during the revision process?
No. At 4M, we prioritize function and confidence from day one. If your existing implant or denture needs to be removed, we provide a custom temporary restoration—so you’ll never leave our office toothless, even during healing.
Does implant revision hurt?
Thanks to local anesthesia, IV sedation, and minimally invasive techniques, most patients report only mild discomfort after surgery. Pain is typically managed with over-the-counter medications, and most people return to normal activities within a few days.
What are my sedation options?
We offer a full range of sedation options, including local anesthesia, oral sedation, and IV sedation. Your comfort and peace of mind are top priorities, especially during procedures involving implant removal or bone grafting.
How long will my new implants last?
With proper care, your new implants can last decades—or even a lifetime. We use materials like titanium and zirconia, known for long-term durability and biocompatibility. Regular follow-ups, cleanings, and at-home oral hygiene are key to maximizing the lifespan of your implant-supported restoration.
From Failure to Forever—Start Your Revision Journey Today
If you’re living with pain, uncertainty, gum recession, or dissatisfaction from failed implants, now is the time to take control. At 4M Dental Implant Center, we don’t just correct problems like peri implantitis and bone loss—we create lasting solutions that restore function, aesthetics, and confidence.
Our minimally invasive implant restoration protocol is grounded in cutting-edge diagnostics, advanced surgical techniques, world-class materials, and compassionate care. Whether you’re correcting a failed mini dental implant, managing complications from a previous implant surgery, upgrading from dentures, or seeking ridge preservation and bone graft support, we’re here to help.
Every dental procedure is designed with precision—from soft tissue management and implant placement to oral surgery and bone regeneration when necessary. Our goal is to ensure that your dental prosthesis not only looks natural but also performs flawlessly for years to come.
Schedule your free 4M Smile Assessment today and learn how minimally invasive surgery can transform your oral health and confidence.
Don’t settle for discomfort or disappointment. Get the smile you deserve—permanently, with the right balance of technology, experience, and care.
Schedule Your Free Consultation





Reader Interactions