When it comes to replacing missing teeth, durability and long-term performance matter just as much as aesthetics; that’s why titanium dental implants have remained the gold standard in implant dentistry for decades. With unmatched strength, superior biocompatibility, and exceptional corrosion resistance, titanium implants are designed to last, often doing so for decades when placed and properly maintained.
At 4M Dental Implant Center, we place only high-quality titanium implants with precision using 3D imaging, digital planning, and custom prosthetics. Our approach ensures that every implant post, abutment, and crown works in harmony with your jawbone, bite, and overall oral health.
Whether you’re exploring your first dental restoration or researching alternatives to bridges and dentures, this guide will help you make an informed, confident decision regarding titanium alloys for implants and know why they are trusted by dental professionals worldwide.
We’ll cover how titanium performs under real-world conditions, the science behind its success, and how to maintain your implants for lifelong function and beauty.
What Are Titanium Dental Implants?
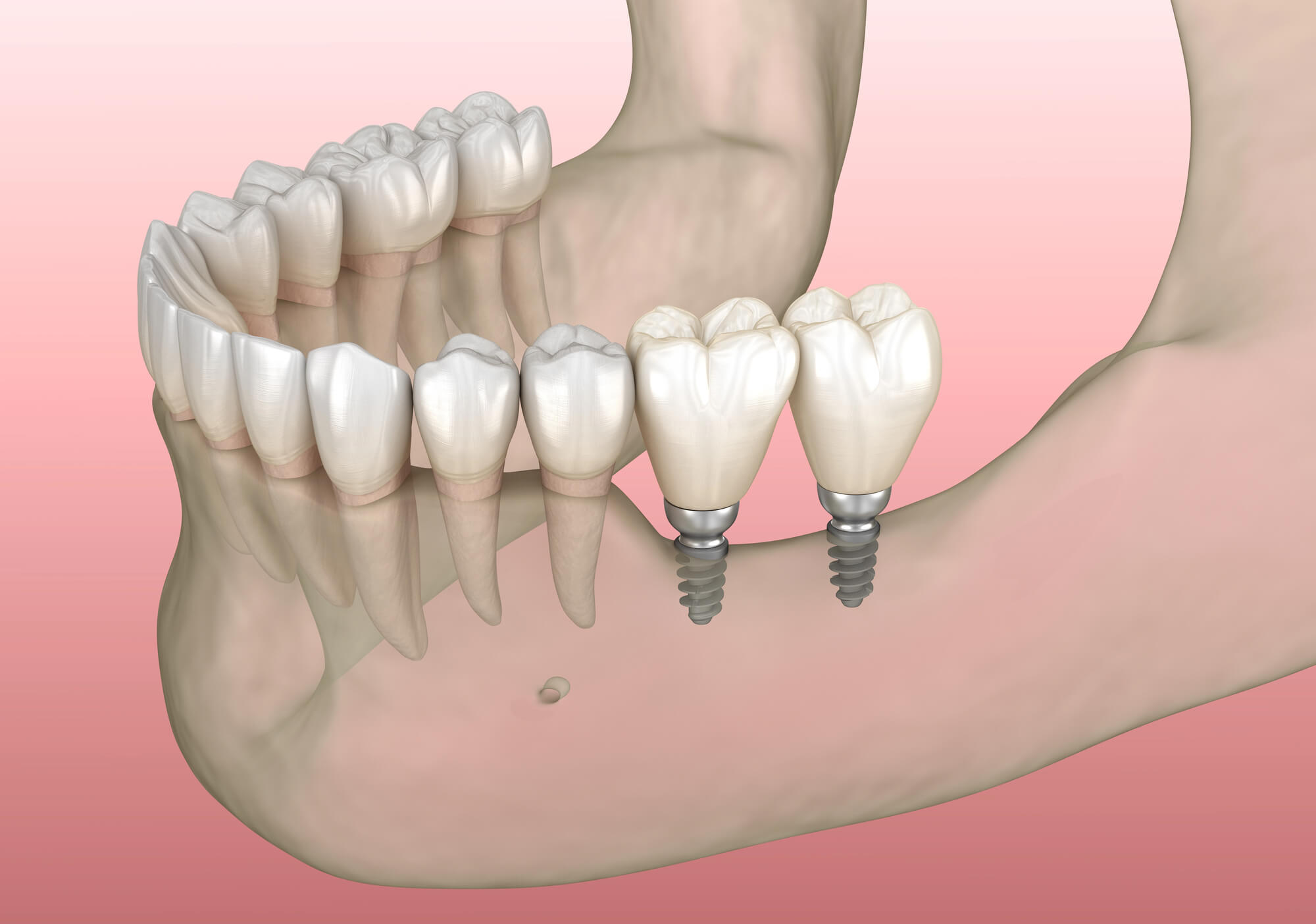
Titanium dental implants are prosthetic devices designed to replace missing teeth by integrating directly into the jaw bone. Each implant typically consists of three main parts:
- The implant post (or implant screw), made of medical-grade titanium or titanium alloys, acts as the artificial root
- The abutment, which connects the post to the restoration
- The visible dental crown, designed to mimic the look and function of a natural tooth
Together, these components form a stable and natural-looking solution for single-tooth replacements, implant-supported bridges, and full arch or All-on-X dental solutions.
Why Titanium?
Titanium is the material of choice in modern dental implantology due to its:
- High strength-to-weight ratio
- Outstanding biocompatibility
- Resistance to corrosion, including pitting corrosion, crevice corrosion, and galvanic corrosion
- Long-standing track record in both dentistry and orthopedics
The key to its longevity lies in its titanium oxide layer, a naturally forming film that protects the implant from corrosive elements in the mouth, such as acidic foods, low oral pH, or saliva-related ions.
How Titanium Implants Are Placed
The implant placement process is a carefully orchestrated surgical procedure. For example, at 4M, we use:
- 3D imaging and bone density assessments to map your anatomy
- Virtual planning software to determine ideal implant positions
- Surgical guidance protocols to enhance precision and minimize healing time
Thanks to our experienced and trained implant dentists, your implant is designed to function like a natural tooth root, providing unmatched stability and helping to prevent bone loss over time.
Why Titanium Is the Gold Standard for Implant Durability
When patients ask, “How long do dental implants last?” the answer is often decades, which is even truer when those implants are made of titanium. Titanium implants are engineered to withstand a lifetime of biting, chewing, and daily wear, offering both functional strength and long-term resilience in even the most demanding conditions.
Mechanical Strength and Masticatory Force Resistance
Titanium’s mechanical properties make it ideal for handling the masticatory forces (biting and chewing pressure) placed on teeth. Whether you’re eating crunchy vegetables, steak, or nuts, titanium’s tensile strength allows it to perform without fracturing, unlike some ceramic alternatives.
Its flexibility and resistance to micro-movements also make it especially effective in supporting multi-unit bridges and full-mouth restorations, where load distribution is critical.
Corrosion Resistance in the Oral Environment
The oral cavity is a challenging environment for most implant materials: It’s moist, variable in pH, and filled with bacteria and acids. Titanium’s corrosion resistance, thanks to the titanium oxide layer, is a key reason for its success in implant surgery. This protective layer defends against:
- Pitting corrosion from dental plaque or acidic exposure
- Crevice corrosion at the connection points between the abutment and the implant
- Galvanic corrosion when in proximity to other metals (e.g., amalgam or gold fillings)
When maintained with proper oral hygiene, including daily brushing, flossing, and routine dental check-ups, these implants resist degradation and remain structurally sound for decades.
Backed by Research and Long-Term Success
Studies consistently show titanium implants achieve long-term success rates above 95%, especially when supported by proper implant placement, regular dental maintenance, and healthy bone tissue. These results make them a clear choice for patients seeking a lifelong solution to tooth loss.
Osseointegration: Titanium’s Secret to Longevity
One of the defining strengths of titanium dental implants is their ability to fuse with the jawbone through a process called osseointegration.
How Osseointegration Works
After implant placement, the surrounding bone tissue begins to grow and bond directly to the surface of the titanium implant post. This fusion process, known as osseointegration, creates a stable foundation that functions like a natural tooth root.
Titanium’s unique surface properties and the protective titanium oxide layer encourage this bonding. Modern implant designs often incorporate surface enhancements, such as sandblasting or acid etching, to enhance contact between the implant and bone tissue, thereby improving integration and reducing healing time.
Reducing the Risk of Implant Failure
Because osseointegration is essential for implant success, its strength directly affects long-term outcomes. When integration is successful:
- The implant can support strong biting (masticatory forces) without loosening
- The surrounding jawbone stays stimulated, helping prevent bone loss
- The risk of implant failure due to micro-movements or instability is significantly reduced
At 4M, we utilize advanced diagnostics—including bone density assessments and 3D imaging—to ensure the bone is healthy and sufficient for successful osseointegration before proceeding with any surgical procedure.
Precision and Planning Matter
The material matters, but successful osseointegration ultimately is about execution. That’s why we use virtual planning software and expert clinical protocols to position each titanium implant at the ideal angle, depth, and bone zone. This ensures strong integration and optimal long-term performance.

Biocompatibility and Health Benefits of Titanium Implants
Beyond strength and integration, titanium implants offer another critical advantage: they are remarkably well-tolerated by the human body. Their biocompatibility plays a major role in healing, comfort, and long-term oral health.
Compatibility with Bone and Gum Tissue
Titanium’s natural compatibility with both hard and soft tissues makes it the material of choice for implant dentistry. Unlike materials that may trigger immune responses or rejection, titanium is widely accepted by the body and integrates smoothly into the jawbone without irritating the surrounding gum tissue.
This is particularly important for patients with sensitive gums or those prone to inflammation. The titanium oxide layer protects the implant from corrosion and helps ensure a healthy tissue response over the long term.
Low Risk of Allergic Reaction
Not only is it a biocompatible material, but titanium is also considered hypoallergenic for most patients. However, in rare cases where metal sensitivity is a concern, allergy testing may be recommended. Fortunately, the vast majority of patients experience no adverse reactions to titanium or titanium alloys used in dental implantology.
If you have a history of metal allergies, the 4M team will work with you during your consultation to evaluate your medical background and recommend a solution tailored to your needs.
Supporting Long-Term Oral Health
With the missing tooth roots replaced and proper bite alignment restored, thanks to the titanium dental implants, patients also regain healthy chewing function and preserve surrounding teeth. They also reduce the risk of bone loss by stimulating the jawbone, something that dentures and bridges alone cannot do.
With proper oral hygiene, including brushing, flossing, and regular dental check-ups, titanium implants can support lifelong oral health with minimal complications.
Aesthetic Outcomes and Prosthetic Versatility
While strength and integration are foundational, aesthetics also matter. Titanium dental implants offer the structural support needed to deliver beautiful, lifelike smiles through custom dental restorations. When combined with expertly crafted crowns or bridges, the result is both functional and natural-looking.
Abutments and Crown Compatibility
Titanium implants are compatible with a wide range of prosthetic options. Once the implant has fully integrated into the jawbone, a titanium or zirconia abutment can be placed on top. This component serves as the connector between the implant root and the visible crown.
Whether you’re replacing a single tooth, multiple teeth, or undergoing a full mouth restoration, titanium implants support:
- Custom ceramic or, the preferred 4M choice, zirconia crowns
- Implant-supported bridges
- Full arch restorations like All-on-X systems
These restorations are color-matched to your natural teeth, designed for proper bite alignment, and shaped to complement your facial features and gum line.
Tailored for Aesthetic Appeal
A major concern in implant dentistry is how the final result looks in the smile zone. Titanium posts are placed beneath the gum tissue, and the visible portion of the restoration (the crown) is made of ceramic or zirconia. This means you get all the strength of titanium with none of the metallic appearance.
In patients with thin gum tissue, special care is taken to avoid any gray shine-through. Our digital planning and prosthetic customization processes ensure that each restoration looks as good as it feels.
Precision Craftsmanship from Lab to Chair
At 4M, we work closely with dental laboratory technicians to fabricate restorations that meet both aesthetic and functional standards. Through 3D imaging, intraoral scans, and detailed case planning, each dental crown or prosthetic is designed for precision fit and long-term success.
Titanium Implants with Zirconia and Ceramic Restorations
At 4M Dental Implant Center, we exclusively use titanium for implant posts due to its unmatched strength, integration ability, and proven clinical success. But when it comes to the visible part of your restoration, the crown or bridge, we often use zirconia or a titanium bar with milled PMMA for enhanced appearance and durability.
Strength from the Foundation Up
Titanium serves as the structural base for your implant, embedded deep into the jawbone. Its load-bearing capacity allows it to support even the most complex dental restorations, including:
- Single tooth replacements
- Multi-unit bridges
- Full arch rehabilitations
Once the titanium implant has successfully osseointegrated, it provides a strong foundation for high-performance prosthetics.
Aesthetics Where It Matters
Zirconia and ceramic materials are used in the fabrication of the visible portion of the restoration, your dental crown or bridge. These materials:
- Mimic the color and translucency of natural teeth
- Resist staining and wear
- Work harmoniously with gum tissue for natural contours and healthy margins
This combination of titanium for the implant post and zirconia or ceramic for the crown delivers both strength and visual appeal, especially important for patients prioritizing a natural-looking smile.
Seamless Integration for Function and Beauty
By using titanium implants with zirconia restorations, we offer patients the best of both worlds: reliability beneath the surface and beauty above it. The result is a long-lasting, custom-engineered dental solution that restores function, enhances appearance, and supports overall oral health.

How Titanium Implants Support Full-Mouth and Complex Restorations
Titanium implants aren’t just for single tooth replacements. They’re engineered to handle the demands of complex dental restorations and full arch solutions. Their strength, durability, and osseointegration capacity make them ideal for long-span bridges and All-on-X treatments.
Built for Full Arch and All-on-X Systems
Titanium dental implants are commonly used in full arch procedures like All-on-Four or All-on-Six, where four to six implants support an entire set of upper or lower teeth. In these cases, each titanium implant post acts as an anchor, distributing bite force evenly and minimizing stress on the jawbone.
The precision of titanium placement allows for:
- Fewer implants to support more teeth
- Reduced the need for bone grafting in many cases
- Immediate load capabilities in certain treatment protocols
Supporting Bridges and Multi-Tooth Restorations
For patients missing several adjacent teeth, titanium implants can also support fixed bridges. Unlike traditional bridges that rely on natural teeth for support (which can weaken them over time), implant-supported bridges transfer force directly to the jawbone, promoting better long-term oral health.
This level of structural integrity is only possible with materials like titanium that can withstand years of masticatory forces without fracturing or degrading.
Stability for Long-Term Function and Comfort
Whether used for a single crown or full mouth rehabilitation, titanium implants provide a stable, secure foundation that mimics the function of natural teeth. With proper planning and precise placement, they support lasting function, enhanced speech, and comfort without slippage, irritation, or dietary restrictions associated with removable dentures.
Factors That Influence Implant Longevity
While titanium dental implants are built to last, their lifespan is also influenced by several patient- and procedure-specific factors. At 4M Dental Implant Center, we provide comprehensive guidance to maximize the lifespan of your implants and restorations.
Oral Hygiene and Maintenance
Daily brushing, flossing, and routine dental check-ups are essential to prevent plaque buildup, gum inflammation, and peri-implant disease. Even though titanium resists corrosion, poor oral hygiene can lead to gum issues and bone loss around the implant, increasing the risk of failure.
We recommend:
- Consistent at-home care using soft-bristle toothbrushes and non-abrasive toothpaste
- Professional dental cleanings every 3–6 months
- Periodic monitoring of implant health and surrounding tissues
Proper Surgical Planning and Placement
The long-term success of titanium implants begins before the first incision. Our team uses digital planning tools, 3D imaging, and other techniques to ensure optimal angulation, depth, and bone engagement during implant placement. Poor alignment or shallow insertion can compromise osseointegration and increase mechanical stress over time.
Systemic Health and Lifestyle Factors
Certain health conditions and lifestyle habits can also affect implant longevity:
- Smoking and uncontrolled diabetes increase the risk of bone complications and gum disease.
- Poor diet or high consumption of acidic foods can disrupt oral pH and contribute to soft tissue inflammation.
- Untreated bone problems or low bone density may limit support around the implant site.
During your consultation, we’ll evaluate your medical history, conduct bone density assessments, and create a plan that’s tailored to your health profile.
The 4M Dental Implant Center Difference
When you choose 4M Dental Implant Center, you’re choosing a team of experienced implant dentists, oral surgeons, and restorative professionals who understand the science, art, and precision required for successful implant outcomes.
- Our Commitment to High-Quality Implants: We exclusively use premium-grade titanium implants with proven clinical track records. Our implant systems are chosen for their mechanical strength, corrosion resistance, and advanced surface designs that promote rapid and reliable osseointegration.
- Advanced Technology, In-House Coordination: From 3D imaging and virtual planning to in-house dental labs and prosthetic fabrication, our fully integrated process ensures every phase of treatment is carefully coordinated for optimal outcomes.
- We Specialize In: Immediate load protocols when clinically appropriate, full arch and complex reconstructions, and custom abutments and implant crowns for natural aesthetics.
- Patient-Centered Results: Every treatment plan at 4M is personalized. We prioritize not just clinical success, but long-term satisfaction, aesthetics, and function. We’ll walk you through every detail, from costs and materials to maintenance and aftercare, so you feel informed, confident, and empowered every step of the way.
Is Titanium Right for You? How to Know
If you’re considering a dental implant, titanium dental implants are almost always the preferred option, especially when durability of titanium implants, integration with human bone, and long term success are top priorities in implant dentistry. Titanium implants offer exceptional corrosion resistance, strong mechanical properties, and proven biocompatibility titanium that supports implant success inside the human body. Still, like any medical procedure or surgical procedure, outcomes depend on proper surgical planning, careful implant placement, and individual oral health factors that dental professionals evaluate closely.
Ideal Candidates for Titanium Dental Implants
You may be a strong candidate if you:
Have one or more missing teeth or tooth loss requiring dental restoration or replacing missing teeth with a replacement tooth that functions like a natural tooth
Have sufficient jawbone, healthy bone quality, or are open to bone reconstruction, soft tissue grafting, or bone density assessments to support bone integration
Are in good general and oral health, with healthy gum tissue, soft tissue, and surrounding tissues at the implant site
Can commit to proper oral hygiene, dental maintenance, and regular dental check ups to protect implant health and reduce implant failure risk
Titanium contributes to clinical success because titanium remains stable, titanium resists corrosion, and titanium alloys used in high quality implants integrate predictably with bone cells during the healing process. Even if you’ve been told you’re not a candidate elsewhere due to bone density, poor oral hygiene history, or concerns about implant materials, 4M’s advanced implant technology, surface treatments, and digital planning may open new options, including single tooth replacements, posterior regions, or cases involving adjacent teeth.
How 4M Determines the Right Solution for You
Our process begins with a comprehensive consultation that reflects modern dental implantology and clinical practice, including:
Medical and dental history review to identify side effects, adverse reactions, allergic reactions, or prior dental procedures
3D imaging, bone density analysis, bone density assessments, and evaluation of surrounding bone tissue and surrounding bone at the implant root location
Personalized treatment plans that align implant materials, implant surface characteristics, implant screw design, titanium post selection, zirconia abutment options, dental crown materials, implant bars if needed, and overall implant placement process
We carefully evaluate the implant site, gum tissue, soft tissue inflammation risks, bone quality, and surface characteristics to select the right artificial tooth root, implant root, and dental crown. We also compare options such as titanium implants vs zirconia implant, zirconium implants, zirconia dental alternatives, and ceramic alternatives when appropriate, ensuring optimal implant longevity, structural integrity, and patient outcomes.
Schedule Your Consultation Today
Ready to restore your smile with one of the most reliable dental solutions available? Titanium implants make titanium implants a leading choice in implant dentistry due to corrosion resistance, biocompatible material properties, and proven long term success. Contact 4M Dental Implant Center to schedule your consultation with experienced oral surgeons and dental professionals.
Our team will explain the implant placement process, answer questions about implant success, implant longevity, implant materials, implant technology, implant bars if needed, and guide you through every step—from evaluation to final dental restoration.
You can call us, send a message, or submit your details by email—we’ll take it from there and help you achieve strong, healthy results that support your overall oral health.