Dental implant surgery has become one of the most reliable dental treatments in modern implant dentistry, with success rates exceeding 99% when proper surgical techniques, treatment planning, and patient cooperation are followed. Despite this high success rate, dental implant complications can still occur. These complications are not necessarily a reflection of the skill of the dental professional or surgeons involved.
Instead, they may arise from individual patient factors, medical conditions, healing responses, or extremely rare issues with materials such as the titanium screw, zirconia abutment, or prosthesis.
This guide explores the most common dental implant complications, their risk factors, and how they are treated or managed. It will also highlight the importance of proper jaw preparation, careful surgical protocol, and diligent post-surgical healing to ensure every artificial tooth, dental crown, or dental bridge supported by implants remains stable for years to come.
Why Talk About Dental Implant Complications?
For patients, it’s important to understand that while dental implants provide strong support from the bone and function as a permanent replacement for missing teeth, complications can develop if the surgical procedure or post-surgical aftercare is disrupted.
Conditions like peri-implantitis, bone loss, nerve damage, or sinusitis may develop due to poor oral hygiene, gum disease, smoking, or systemic medical conditions like diabetes, osteoporosis, or autoimmune disorders.
Recognizing risk factors early allows patients to partner with their dental surgeon in prevention and treatment.
What Are Dental Implant Complications?
Dental implant complications are any issues that interfere with the healing, stability, or long-term success of a dental implant after the surgical procedure. While dental implant surgery is designed to replace a missing tooth with a titanium implant post anchored in the jaw bone, complications can affect the integration process known as osseointegration.
When osseointegration is disrupted, the implant may fail to fuse properly with the bone, leading to implant mobility, discomfort, or eventual implant failure.
Complications can be grouped into two main categories:
- Short-term complications – These occur shortly after implant placement and may involve infection at the implant site, sinus damage in the maxillary sinus, very rare allergic reactions to dental implant metal, rejection of the titanium screw, or problems with sedation or anesthesia. In rare cases, patients may develop swelling, bleeding, or nerve-related symptoms if the inferior alveolar nerve or trigeminal nerve is affected during surgery.
- Long-term complications – These usually appear months or years after dental surgery. They include peri-implantitis (infection around the implant and gum line), progressive bone loss, loose implants due to insufficient bone density, or mechanical problems with the dental crown, prosthesis, or dental bridge placed on top of the implant. Long-term issues may also include sinus issues if the Schneiderian membrane was compromised during maxillary sinus surgery or sinus lift procedures.
Dental implant complications can arise from multiple factors; however, with proper planning, the use of 3D images for surgical planning, and adherence to surgical protocol, many of these complications can be avoided or treated successfully if they occur.
The Most Common Dental Implant Complications
Even with careful treatment planning, advanced surgical techniques, and experienced dental professionals, complications can occur after dental implant surgery. Below are the most common issues patients may face, along with causes, symptoms, and treatment approaches.
Infection and Peri-Implantitis
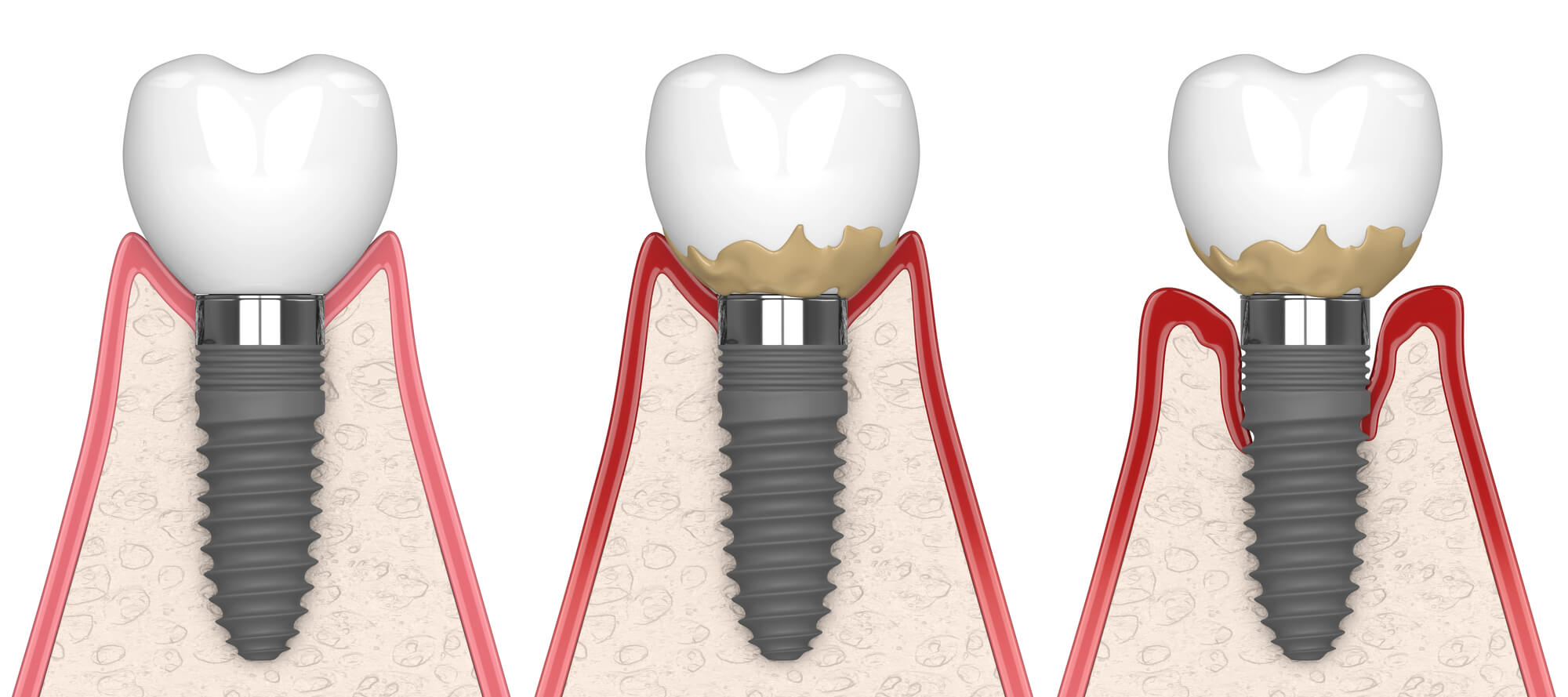
One of the most common complications following implant placement is infection at the implant site. Peri-implantitis is a condition where bacteria accumulate around the gum line and titanium screw, leading to inflammation, bone loss, and potential implant failure.
- Risk factors: poor oral hygiene, untreated gum disease, smoking, diabetes, or autoimmune disease.
- Symptoms: redness, swelling, tenderness, bleeding gums, or pus near the implant.
- Treatment: early-stage infection may be treated with professional cleaning, antibiotics, and antibacterial rinses; advanced cases may require surgical procedures like bone grafting or implant replacement.
Implant Failure and Lack of Osseointegration
Dental implants rely on osseointegration, which is the natural process where the titanium implant post fuses with the jawbone. If this does not occur properly, dental implant failure can result.
- Causes: low bone density, poor surgical protocol, medical conditions like osteoporosis or rheumatoid arthritis, smoking, or allergic reactions to implant metal.
- Signs: implant mobility, persistent pain, or a loose implant that fails to provide stable support for the prosthesis.
- Solutions: bone grafting or ridge augmentation to improve jaw preparation, replacing the implant, or addressing systemic medical conditions before re-attempting implant placement.
Bone Loss Around the Implant
Even if bone fusing is successful after the implant procedure, bone loss can still occur as a long-term complication and weaken implant support from the bone, threatening stability. It may occur gradually, sometimes unnoticed by the patient until the implant becomes loose.
- Causes: peri-implantitis, excessive bite force, poor oral hygiene, gum disease, or inadequate jaw preparation.
- Treatment: scaling and root planning, guided tissue regeneration, or bone grafting to restore bone density and support for the artificial tooth.
Nerve Damage
Improper implant placement in the lower jaw can cause nerve damage, especially to the inferior alveolar nerve or trigeminal nerve.
- Symptoms: numbness, tingling, pain, or altered sensation in the lips, tongue, or chin.
- Prevention: using CBCT 3D images for precise treatment planning and adhering to strict surgical protocol.
- Management: nerve damage may resolve over time, but in some cases, surgical correction is required.
Sinus Complications
For implants placed in the upper jaw, there is a risk of sinus complications if the implant protrudes into the sinus cavity or damages the Schneiderian membrane.
- Causes: insufficient jawbone height or inadequate bone density in the maxillary sinus area.
- Complications: sinusitis, sinus infections, or chronic sinus issues.
- Treatment: sinus lift procedures, bone grafts, or surgical correction to reposition or replace the implant.
Mechanical or Prosthetic Complications
Even when the implant integrates successfully, the artificial tooth or dental crown may experience problems.
- Examples: chipped porcelain crowns, fractured zirconia, loose abutments, or instability in a dental bridge or denture attached to implants.
- Causes: bite stress, faulty materials, or a misfit prosthesis.
- Solutions: replacement of the dental crown, adjustment of bite alignment, or reinforcement of the prosthesis with stronger materials.
Risk Factors That Increase Complications
Although dental implant surgery has a very high success rate, certain patient-specific or procedural factors can increase the likelihood of dental implant complications. Identifying these risks early allows both the dental surgeon and patient to take preventive steps.
Smoking and Poor Oral Hygiene
Smoking restricts blood flow, delays healing at the implant site, and weakens support from the bone. Combined with poor oral hygiene, it increases the risk of peri-implantitis, gum disease, and eventual implant failure. Patients who smoke should quit before undergoing implant placement and commit to strict oral care after the surgical procedure.
Medical Conditions and Systemic Health Issues
Chronic illnesses such as diabetes, autoimmune disorders, rheumatoid arthritis, and osteoporosis can interfere with osseointegration and bone density. Autoimmune disease and other systemic conditions compromise the immune response, making infection more likely and reducing long-term implant stability. Careful treatment planning, including coordination with a patient’s medical provider, is essential.
Gum Disease and Pre-Existing Oral Health Issues
Untreated gum disease or infection near the gum line increases the risk of peri-implantitis and bone loss. Patients with gum disease should undergo treatment before dental implant surgery to reduce complications and improve implant success.
Low Bone Density or Inadequate Jawbone Support
If the jawbone lacks sufficient density or height, the implant may not achieve stable support. This is especially common in the posterior maxilla near the sinus cavity. Bone grafting, ridge augmentation, or sinus lift procedures may be necessary to create adequate support for the titanium screw or zirconia implant post.
Inexperienced Surgical Technique
Dental implant complications may also occur due to errors in surgical techniques, such as damaging the inferior alveolar nerve, improper jaw preparation, or violating the maxillary sinus or Schneiderian membrane. Working with experienced dental and maxillofacial surgeons who follow strict surgical protocol significantly reduces these risks.
Patient Age and Healing Capacity
Older patients may experience slower healing times due to reduced bone density, chronic medical conditions, or decreased immune response. While patient age alone is not a contraindication for dental implants, it can influence recovery and long-term implant stability.
Early Warning Signs of Dental Implant Failure or Complications
Not every ache or change in your mouth means an implant is failing, but certain signs may indicate problems with implant placement, bone integration, or surrounding gum tissue. If you experience any of the following, it’s best to contact your dental professional or oral and maxillofacial surgeon promptly. Early intervention can make a big difference in preserving your dental implants.
- Persistent Pain or Throbbing: Mild discomfort after dental implant surgery is normal, but intense or worsening pain may suggest issues with osseointegration, surrounding tissue pressure, or even nerve damage near the inferior alveolar nerve or trigeminal nerve.
- Swelling, Redness, or Inflammation: Some swelling is part of the natural healing process, but prolonged gum inflammation, redness, or bleeding around the implant post can indicate peri-implantitis or infection at the implant site.
- Loose Implant or Wiggling Sensation: A properly placed titanium or zirconia implant should feel as secure as a natural tooth once healed. If your implant feels mobile, it may point to implant overload, bone loss, implant screw issues, or incomplete fusion with the jawbone.
- Gum Recession or Visible Threads of the Implant: If gum tissue pulls back and you notice exposed metal threads near the gum line, it could be a sign of gum disease, bone deterioration, or failing support from the bone around the implant.
- Difficulty Chewing or Biting Down Normally: Pain or discomfort while chewing—especially on harder foods—can suggest implant misalignment, implant mobility, or insufficient jaw preparation during the surgical procedure.
- Bad Taste or Odor: A persistent bad taste or foul odor in the mouth may indicate bacterial infection, poor oral hygiene around the implant, or peri-implantitis.
- Fever or General Malaise: In rare cases, untreated infection around an implant can cause systemic symptoms like fever, fatigue, or malaise. This requires immediate evaluation by a dental surgeon to prevent further complications.
Recognizing these signs early doesn’t always mean implant failure is inevitable, but it does mean you should act quickly. With timely treatment, many complications can be reversed, preserving your implant and protecting your long-term oral health.
How to Treat and Manage Dental Implant Complications
When dental implant complications occur, prompt diagnosis and treatment are essential to preserve the implant, protect surrounding bone and gum tissue, and maintain long-term oral health. Management strategies vary depending on the type and severity of the complication.
Early Detection Through Regular Follow-Ups
Routine checkups with a dental professional after implant placement are critical. Dental surgeons use clinical exams, X-rays, and 3D images to detect peri-implantitis, bone loss, or implant mobility early. Catching complications early often means simpler, non-surgical treatment.
Non-Surgical Treatments
Minor infections around the implant site can often be treated without additional surgery. Approaches include professional cleaning, antibiotic therapy, and improved oral hygiene practices to reduce bacteria at the gum line. For prosthetic complications, such as a loose dental crown or fractured zirconia prosthesis, simple repairs or adjustments may resolve the problem.
Surgical Interventions
More advanced complications sometimes require corrective surgical procedures:
- Bone grafting or ridge augmentation can rebuild jawbone density when bone loss threatens implant stability.
- Sinus lift surgery may correct issues in the maxillary sinus cavity or Schneiderian membrane.
- Implant replacement or revision is sometimes necessary if the titanium screw or implant fails to integrate with the jaw bone, leading to dental implant failure.
Compliance With Surgical Protocol
Following all post-surgical instructions, including prescribed medications, use of ice packs, and rest recommendations, is essential. Patients should also avoid strenuous activity immediately after dental surgery, as this may interfere with healing and implant stability.

Proper Aftercare to Prevent Complications
Successful management of complications depends not only on the dental surgeon but also on the patient. Quitting smoking, controlling medical conditions like diabetes, and practicing excellent oral hygiene are critical steps in reducing the risk of recurrent issues.
Following the surgical protocol, including recommended restrictions after surgery, helps ensure long-term success.
- Daily Oral Hygiene: Keeping the implant site clean is essential to prevent peri-implantitis and bone loss. Patients should brush gently around the gum line, floss daily, and use antibacterial rinses as recommended by their dental professional. Avoiding plaque buildup is one of the most effective ways to protect osseointegration and long-term implant stability.
- Lifestyle Choices and Habits: Smoking is one of the strongest risk factors for implant failure because it reduces blood flow, slows bone healing, and increases the likelihood of infection. Excessive alcohol consumption also delays recovery. Patients should avoid smoking and minimize alcohol intake during healing to protect the titanium screw and post, and surrounding jaw bone.
- Nutrition and Healing Support: A soft-food diet immediately following the surgical procedure helps protect the implant site. Nutrient-rich foods that support bone health, such as those high in calcium and vitamin D, promote osseointegration and stability of the implant post. Hard or sticky foods should be avoided until the dental surgeon confirms the implant is secure.
- Professional Follow-Ups and Maintenance: Regular visits to the dental surgeon are critical. These appointments allow professionals to monitor bone density, check for implant mobility, and ensure the dental crown, prosthesis, or dental bridge is fitting correctly. Professional cleanings reduce bacterial risk at the gum line and around the implant.
Awareness, Prevention, and Lasting Success
Dental implant surgery is one of the most successful and predictable dental treatments available, with success rates above 99%. Still, complications such as peri-implantitis, bone loss, implant mobility, nerve damage, or sinus issues can occur in certain situations. Factors like bone density, gum disease, smoking, and systemic medical conditions such as diabetes or autoimmune disorders influence these risks.
With proper treatment planning, advanced surgical techniques, and patient cooperation in post-surgical aftercare, most dental implant complications can be prevented or effectively managed.
At 4M Dental Implant Center, our dental professionals follow strict surgical protocols and use advanced imaging, 3D treatment planning, and state-of-the-art surgical techniques to ensure stability, osseointegration, and long-lasting results.
If you’re considering dental implants—or need help restoring confidence in your smile—schedule a consultation with 4M today and take the first step toward a healthier, brighter future.
Frequently Asked Questions About Dental Implants Complications
What are the most common dental implants complications?
Dental implants complications may include infection at the implant site, peri-implantitis, bone loss, nerve injury, and implant fractures. Problems with implant placement or improper implant surgery can also cause inflammation and bone loss around the implant. These issues may develop shortly after the dental implant procedure or years later as long-term potential complications.
What risk factors can increase the chance of dental implant failure?
Implant failure is often linked to poor oral hygiene, gum disease, smoking, autoimmune disorders, osteoporosis, or other medical conditions that interfere with bone healing and blood flow. Insufficient bone density, improper implant placement, or teeth grinding may also increase the risk of complications. Patients with unhealthy gums or existing teeth problems should address them before dental implant surgery to minimize risks.
How do dental implants work to replace missing teeth?
Dental implants act as a permanent tooth replacement option. During the dental implant procedure, an oral surgeon or maxillofacial surgery specialist places a titanium metal post into the surrounding bone of the upper jaw or lower jaw. As new bone growth occurs, the implant fuses with the jaw through osseointegration, supporting an artificial tooth, dental crown, or replacement tooth. This makes dental implants function like natural teeth while protecting other teeth and maintaining bone density.
What can patients do to improve healing after implant surgery?
After implant treatment, patients should follow their surgeon’s instructions to ensure a smooth healing process. Eating soft foods, practicing good oral hygiene, and avoiding smoking or alcohol will support bone growth and reduce the risk of infection at the implant site. Using antibacterial rinses and keeping the surgical site clean helps prevent plaque buildup and gum tissue inflammation. Regular follow-ups with an experienced dentist or oral and maxillofacial surgery specialist help detect potential risks early.
How can dental implant complications be treated or prevented?
If a dental implant fails due to bone loss, gum disease, or improper placement, treatments may include a bone graft, sinus lift for the sinus cavity, or replacement of one implant with a new dental implant placement. Managing lifestyle factors, reviewing medical history, and ensuring sufficient bone density are key steps in minimizing risks. With careful implant procedure planning, an experienced dentist, and proper aftercare, most dental implants work successfully and provide long-lasting results in replacing missing teeth.

