Techniques and innovations around surgical implant placement make patient-focused, minimally invasive dental care almost standard now, especially when being treated by experienced professionals like those at 4M.
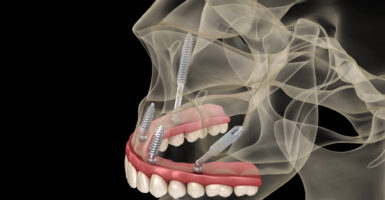
In few areas is this evolution more evident than the choice between flapless and flapped surgical techniques in dental implant therapy. Both approaches are widely used in modern implantology, but they differ significantly in technique, visibility, soft-tissue management, and long-term clinical outcomes.
With digital technologies like 3D imaging and minimally invasive protocols reshaping the field and making flapless implantology an increasingly viable solution, there’s growing debate about its use versus open-flap surgical techniques. While flapless surgery is often praised for reducing post-surgical pain, improving wound healing index scores, and avoiding bone loss, flapped implant placement still allows for greater visibility for surgeons and control over anatomical variations and anomalies like bone fenestrations, ridge width, and vertical height.
In this comprehensive comparison, we’ll explore the benefits, limitations, and data-supported performance of both the flapless technique and flapped surgical methods, including how they influence marginal bone loss, aesthetic parameters, and patient-reported outcomes.
Whether you’re a patient exploring single immediate implant placement or a clinician aiming to optimize implant survival rates, there’s great value in knowing the implications of each technique.
What Are Flapless and Flapped Implant Surgeries?
Flapless and flapped implant surgeries represent two distinct approaches to implant placement, each with its own set of protocols, indications, and impacts on dental implant outcomes.
Flapless Implant Surgery
The flapless technique involves placing the implant directly through the soft tissue without lifting a full-thickness flap to expose the underlying bone. Instead, a tissue punch or small incision is used to create access to the alveolar ridge, followed by immediate drilling and implant installation. This approach is often guided by cone-beam computed tomography (CBCT) or computer-aided surgical guides to optimize placement accuracy and reduce the risk of damaging anatomical structures.
The core benefits of flapless implant surgery include minimal trauma to soft tissue, reduced bleeding and postoperative discomfort, and preservation of crestal bone and periosteal blood supply.
Flapped Implant Surgery
In contrast, flapped implant placement involves making an incision and elevating a mucoperiosteal flap to expose the bone fully. This surgical approach allows for thorough inspection of ridge morphology, management of vertical ridge augmentation, and access for socket grafting or contouring prior to implant placement.
Flapped surgery is considered the gold standard for cases requiring bone grafting or alveolar ridge preservation. And, while flapped procedures may result in slightly longer healing times and greater post-surgical pain, they offer significant advantages in managing anatomic variability and reducing implant failure rates in challenging scenarios.
The Surgical Techniques: Step-by-Step Comparison
While both flapless and flapped procedures are designed to achieve long-term implant success, the surgical process and clinical decision-making involved in each vary considerably.
Flapless Implant Placement
In flapless implant surgery, no full-thickness flap is elevated. Instead, the clinician accesses the alveolar ridge by perforating the soft tissue using a circular tissue punch or a small incision. This minimally invasive access is usually guided by a radiographic surgical template based on cone-beam computed tomography (CBCT) scans to ensure accuracy in implant installation position.
Key features of this surgical approach include:
- Minimal disruption of the soft tissue and vascular supply
- Faster operating time
- Reduced postoperative discomfort and bleeding
- Improved wound healing index and soft tissue aesthetics
This method is often employed in cases with optimal bone volume and density, particularly in single-tooth implants or cases requiring immediate loading. However, the inability to visualize the underlying bone limits intraoperative decision-making. Poor angulation, failure to detect bone fenestrations, or malpositioned implants may compromise implant success, particularly in anatomically challenging sites.
Flapped Implant Surgery
Flapped implant surgery begins with an incision through the soft tissue, followed by elevation of a mucoperiosteal flap to expose the alveolar bone. This open-flap surgical technique enables direct evaluation of bone volume, crest height, and ridge width, allowing the clinician to perform bone reshaping, socket grafting, or guided bone regeneration if needed before placing the dental implant.
Surgical characteristics of this approach include:
- Assessing and correcting crestal bone changes
- Direct handling of bone resorption, ridge width irregularities, or vertical defects
- Greater control in implant positioning and angle correction
- Performing histological analysis or harvesting samples for microbiological outcomes, such as matrix metalloproteinase-8 activity linked to peri-implantitis
Though more invasive, flapped procedures are often required in cases of vertical ridge augmentation, compromised bone quality, or in situations where microbiological analysis (such as measuring the presence of Porphyromonas gingivalis or Tannerella forsythia) is clinically valuable.
Advantages of Flapless Implant Surgery
Flapless implant surgery has gained increasing popularity due to its patient-friendly nature and promising short-term outcomes in suitable cases. The minimally invasive character of the flapless technique offers distinct benefits across several clinical and patient-reported dimensions.
Reduced Surgical Trauma and Discomfort
By avoiding the elevation of a full-thickness flap, flapless implant placement results in less trauma to the periosteum and vascular structures, leading to a lower incidence of post-surgical pain, minimal bleeding and swelling, a decreased risk of postoperative infection, and faster soft tissue healing.
These advantages contribute to higher patient satisfaction and improved scores on the visual analogue scale when compared to traditional flapped surgical techniques.
Preservation of Crestal Bone and Soft Tissue
One of the most frequently cited advantages of flapless surgery is its role in maintaining crestal bone levels. Several randomized controlled trials (RCTs) and systematic reviews suggest that avoiding flap elevation can reduce marginal bone loss and the need for crestal bone remodeling. It can also enhance the soft tissue seal around the implant collar.
This benefit is particularly important for long-term prosthetic rehabilitation outcomes.
Improved Wound Healing and Esthetics
Without the need for sutures or extensive incisions, flapless implant placement allows for better preservation of the soft tissue contour. Healing is typically faster, with a lower risk of scar formation or gingival recession, particularly in cases involving immediate implant placement or anterior single-tooth implants.
Efficient Workflow with Digital Integration
When combined with digital and CBCT-based planning, flapless surgery enables highly accurate placement of implants using surgical guides. This combination reduces surgical time, supports immediate loading protocols, and enhances the predictability of implant positioning, all of which contribute to streamlined clinical outcomes and a more comfortable patient experience.
Schedule Your Free Consultation

Drawbacks and Limitations of the Flapless Technique
While flapless implant surgery offers multiple benefits, it is not universally applicable. The success of this approach depends heavily on preoperative planning, digital tools, and the anatomical suitability of the implant site. Without careful case selection and high-resolution radiographic planning, flapless placement carries significant risks.
Limited Visual Access to Bone and Surrounding Structures
One of the most well-documented limitations of the flapless technique is the lack of direct visibility to the underlying bone. This visual restriction can increase the risk of implant placement outside the ideal installation position, mask bone loss or fenestrations, which then results in inadequate assessment of vertical ridge height or buccal plate thickness.
This is especially critical in cases where CBCT imaging is unavailable or incomplete. Even with radiographic planning, tactile feedback may not always reveal subtle irregularities in bone morphology.
Higher Risk of Malposition and Implant Failure in Complex Cases
Flapless surgery is not ideal for sites requiring:
- Bone augmentation
- Socket grafting
- Management of anatomical irregularities
- Extraction sockets with deficient cortical plates
In such cases, attempting a flapless approach may increase implant failure rates. These issues may necessitate removal and revision, particularly in esthetic zones.
Greater Reliance on Imaging and Guided Surgery
Flapless implantology often necessitates cone-beam computed tomography and surgical guides to prevent errors during implant placement. Without this technology, clinicians lack real-time control, especially in anatomically complex areas. Although this can streamline surgery in well-prepared cases, it also increases the dependency on digital tools and may not be feasible in all clinical settings or patient cases.
Limited Soft Tissue Management
Flapless techniques restrict the ability to manipulate or augment soft tissue, which can lead to difficulty managing thick versus thin gingival biotypes and challenges with papilla preservation in the anterior zone.
This is particularly relevant in patients with high esthetic demands, thin soft tissue, or pre-existing periodontal conditions.
Advantages of Flapped Implant Surgery
The flap technique remains the gold standard in many clinical settings, especially when complex bone or soft tissue considerations are involved. The ability to visualize, access, and modify the surgical field provides several technical and clinical advantages that can directly influence long-term implant success.
Direct Visualization of Bone Anatomy
The elevation of a mucoperiosteal flap enables the surgeon to:
- Accurately assess bone quality and morphology
- Measure ridge width and vertical height
- Identify and correct undercuts, fenestrations, or bone resorption
- Adjust implant positioning in real-time
This surgical approach significantly reduces the risk of malpositioned implants and is crucial when planning socket preservation, ridge augmentation, or full-arch restorations.
Better Access for Bone Grafting and Ridge Modification
In cases involving:
- Advanced bone resorption
- Sinus lifting
- Horizontal or vertical ridge augmentation
…flapped access is essential. It allows for accurate placement of grafting materials and membranes, helping to preserve crestal bone and enhance long-term outcomes, particularly when immediate implant placement is not viable.
Enhanced Control of Implant Positioning
The visibility offered by open-flap surgery enables clinicians to optimize the angulation, spacing, and depth of implant placement, which in turn minimizes the risk of cortical perforation or impingement on vital structures.
This results in higher implant survival rates in anatomically challenging cases, as supported by long-term data and numerous RCTs published in medical databases.
Flexibility in Managing Soft Tissue and Aesthetics
In esthetically demanding cases, the flap technique allows for precise contouring of soft tissue, leading to improved aesthetics during healing.
This is particularly valuable in anterior zones (front teeth), full-mouth reconstructions, or patients with gingival asymmetries that would be difficult to manage through a flapless approach.
Drawbacks of the Flap Approach
While flapped implant surgery remains a widely accepted and highly versatile method, especially in complex cases, it also introduces certain drawbacks, particularly in terms of invasiveness, recovery, and potential effects on bone and soft tissue healing.
Greater Surgical Trauma and Patient Discomfort
The creation and elevation of a full-thickness flap involves more soft tissue manipulation than flapless surgery.
This can affect patient-reported outcomes and negatively impact the overall experience, particularly in routine cases that might otherwise benefit from a minimally invasive approach, although an experienced surgeon will be able to keep discomfort and postoperative complications to a minimum.
Risk of Disrupting Crestal Bone Blood Supply
Flap elevation detaches the periosteum from the cortical bone surface, potentially compromising the blood supply that supports the crestal bone. This disruption has been associated in several studies with increased marginal bone loss and a risk of early exposure or soft tissue splintering, especially in patients with thin gums.
These bone-level changes may influence long-term aesthetic outcomes and peri-implant health.
Potential for Increased Bone Resorption
RCTs comparing flapless versus flapped techniques have shown that the open-flap technique may lead to greater initial bone resorption, particularly in the crestal region.
Longer Recovery and More Extensive Aftercare
Patients undergoing flapped procedures generally require sutures and follow-up appointments for suture removal and a longer soft tissue healing period before prosthetic loading.
While these are manageable with proper care, they may lengthen the overall treatment timeline and require additional chair time and patient compliance.

Schedule Your Free Consultation
Clinical Factors That Determine Surgical Approach
The decision between flapless and flapped implant placement isn’t simply a matter of preference, but a function of multiple of the following clinical variables.
Bone Quality and Volume
If cone-beam computed tomography reveals sufficient ridge width and vertical height, flapless surgery may be indicated. However, in cases with:
- Bone loss or low-density
- Thin buccal plates
- Vertical defects
- Irregular ridge contours
…a flapped approach is often safer to ensure precise implant placement and allow for augmentation or bone grafting.
Soft Tissue Thickness and Biotype
Flapless techniques are generally more successful in thick gingival biotypes, where tissue stability and blood supply are better preserved. In thin or highly scalloped tissue, a flapped approach allows for more controlled manipulation, especially when aesthetic parameters must be tightly managed.
Need for Grafting or Ridge Modification
Any scenario requiring:
- Socket preservation
- Guided bone regeneration
- Sinus elevation
- Soft tissue grafting
…will necessitate flap elevation for access and visibility. Attempting flapless placement in such cases increases the risk of implant failure or poor prosthetic outcomes.
Esthetic Demands and Implant Location
In anterior zones or highly visible areas, controlling soft tissue contours is critical. Flapped techniques allow for:
- Papilla preservation
- Augmentation of deficient zones
- Shaping of emergence profiles
For single-tooth implants or full-arch rehabilitations in the esthetic zone, visibility and control matter as much as precision.
Immediate Implant Placement or Loading Protocols
Flapless surgery may support immediate implant placement and immediate loading, especially in posterior zones with ideal bone quality. However, when primary stability is questionable or the socket presents irregularities, a flapped approach is often safer.
Overall Patient Health and Risk Profile
Patients with diabetes, a history of periodontal disease, or previous implant failure may benefit from the enhanced control provided by open-flap surgery, even if it results in slightly longer healing. This also allows for better assessment of peri-implant risk factors, tissue biotype, and microbial exposure.
What the Research Says: Implant Survival Rates and Outcomes
When evaluating any surgical approach in dental implantology, the evidence from randomized controlled trials (RCTs), systematic reviews, and meta-analyses is essential. Research indexed in PubMed/MEDLINE, Cochrane Library, and Web of Science, along with protocols adhering to PRISMA guidelines, offers a comprehensive view of how flapless and flapped surgical techniques compare across various clinical endpoints.
Implant Survival and Success Rates
Numerous RCTs have demonstrated that implant survival rates are statistically comparable between flapless and flapped procedures—particularly in cases involving single-tooth implants or posterior implant sites with adequate bone volume. A 2020 meta-analysis concluded that:
- Flapless and flapped techniques both achieved survival rates >95% over a 3–5 year follow-up period
- Flapless surgery showed slightly higher survival rates in immediate implant placement with proper CBCT planning
However, implant success (which includes esthetics, stability, and soft tissue health) is more dependent on case selection, bone quality, and loading protocols than the surgical approach itself.
Marginal Bone Loss and Crestal Bone Changes
Some clinical trials have reported that marginal bone loss is generally lower in flapless procedures, especially in the first 6 to 12 months post-surgery. This is thought to be due to:
- Preservation of the periosteal blood supply
- Reduced surgical trauma
- Less inflammatory response at the crestal bone level
However, this advantage can be nullified in cases where poor angulation or suboptimal implant installation position occurs due to limited visibility in flapless surgery. Other meta-analyses found that, when accounting for these biases in many of the studies, there truly was no statistically significant difference between the flapless and flap techniques.
Aesthetic and Patient-Reported Outcomes
Flapless surgery tends to score higher in patient-reported outcomes, particularly in:
- Lower post-surgical pain (visual analogue scale)
- Faster return to normal function
- Improved soft tissue esthetics when the biotype is favorable
Conversely, flapped techniques are often favored in anterior esthetic zones when soft tissue contouring is needed.
Microbiological and Immunological Outcomes
Recent studies have begun to explore microbiological outcomes and immunological markers around flapless vs. flapped sites. Notably:
- Sites treated with flapped surgery showed a slightly higher prevalence of Porphyromonas gingivalis and Tannerella forsythia in early healing phases
- Expression of matrix metalloproteinase-8 (MMP-8)—a biomarker for inflammation—was higher in flapped procedures in certain histological analyses.
While still an emerging field, these findings suggest that less invasive surgical approaches may promote a more stable microbiological environment in early healing.

Role of Digital Dentistry and CBCT in Flapless Surgery
The increasing success and safety of flapless implant placement can be directly attributed to the integration of digital dentistry, specifically, cone-beam computed tomography (CBCT), 3D modeling, and surgical guide fabrication.
Enhanced Visualization and Preoperative Planning
CBCT allows for:
- Precise measurement of bone volume, ridge width, and anatomical landmarks
- Evaluation of the relationship between implant sites and adjacent structures (nerves, sinus cavities)
- Detection of potential complications, such as bone fenestrations or concavities, prior to surgery
This radiographic data enables clinicians to virtually place implants and determine whether the patient is a candidate for flapless surgery, long before a scalpel is ever used.
Surgical Guides for Predictable Outcomes
CBCT-based surgical guides improve the safety and accuracy of flapless procedures by:
- Controlling angulation and depth during drilling
- Preventing malposition or cortical perforation
- Supporting immediate loading protocols with high precision
In particular, digitally guided single immediate implant placement in posterior regions has shown high survival rates and minimal marginal bone loss, provided that surgical guides are fabricated based on accurate radiographic and clinical data.
Minimally Invasive Meets High-Tech
Digital workflows now allow for:
- 100% guided flapless implant placement without freehand variation
- Seamless integration with prosthetic planning and restorative outcomes
- Real-time adjustments based on digital wax-ups and occlusal simulations
The convergence of flapless techniques and digital planning has significantly improved the predictability of implant success, particularly in qualified cases.
When Is One Approach Better Than the Other?
There is no universally superior surgical technique in dental implantology, only what’s best for the individual patient and clinical case. Below is a side-by-side breakdown of when each approach is typically favored, based on the current literature, RCT findings, and expert consensus.
| Clinical Scenario | Flapless Implant Surgery | Flapped Implant Surgery |
| Sufficient bone volume and soft tissue | ✅ Recommended | ✔ Possible |
| Minimal surgical trauma is desired | ✅ Ideal | ❌ Less optimal |
| Posterior single-tooth implants | ✅ Strong candidate | ✔ Also viable |
| Immediate implant placement | ✅ Especially effective with CBCT guidance | ✔ May be required if socket defects exist |
| Aesthetic zone with thin tissue biotype | ❌ Risk of poor soft tissue outcomes | ✅ Allows for precise tissue manipulation |
| Ridge augmentation or socket grafting is needed | ❌ Not suitable | ✅ Required |
| High aesthetic demands or gingival asymmetries | ❌ Limited control | ✅ Full access and sculpting possible |
| Poor bone quality, irregular ridge | ❌ Increased risk of misplacement | ✅ Direct access for bone reshaping |
| Need for histological or microbiological sampling | ❌ No access | ✅ Enables analysis |
Ultimately, both surgical approaches can yield excellent outcomes when used appropriately. The key lies in evaluating the patient’s anatomical characteristics, treatment goals, esthetic expectations, and medical history, then selecting the technique that aligns with those variables while maximizing safety and long-term implant success.
What Patients Should Know Before Their Implant Surgery
Whether you’re preparing for your first dental implants, planning immediate implant placement, or seeking a second opinion on implant therapy, understanding your options empowers you to make confident decisions and helps improve dental implant outcomes.
Ask About the Surgical Technique
Don’t hesitate to ask your provider whether they plan to use a flapless implant surgery approach or traditional dental implant surgery involving flap surgery. The decision between flapless or flap surgery should be based on your cone beam computed tomography imaging, the underlying bone quality, peri implant soft tissues, and overall treatment goals—not convenience or habit.
Some patients are ideal candidates for flapless implant placement or transmucosal implant placement, which is associated with minimal surgical trauma and less postoperative discomfort. Others require conventional flapped implant placement or flap elevation due to soft tissue needs, buccal bone augmentation requirements, or alveolar bone limitations. A qualified oral surgery team should clearly explain why one surgical procedure or flap technique is preferred for your implant site.
Review Your Digital Imaging
High-quality diagnostics such as cone beam computed tomography (CBCT) should be part of every modern implant placement evaluation. Your dental team should review these scans with you and explain how adjacent teeth, soft tissue thickness, underlying bone, and crestal bone levels guide surgical implant placement.
This imaging also helps plan for immediately loaded implants, immediate definitive prosthesis installation, or immediate implant function when appropriate.
Understand the Trade-Offs
Every surgical technique has benefits and limitations. Flapless implant placement is less invasive, reduces surgical trauma, and may preserve crestal bone, but requires precise planning and adequate soft tissue and bone support. Flapless implant placement techniques often rely on a tissue punch for transmucosal access, which offers advantages for single tooth implants and selected implant sites.
Conventional implants placed with flap elevation or partial thickness flaps allow greater surgical visibility and control, which can be essential in cases involving bone regeneration, hollow screw implants, buccal bone augmentation, peri implant mucosa challenges, or predominantly soft bone.
Neither approach is universally better; clinical and experimental dentistry literature, including randomized clinical trial data from journals such as Clin Oral Implants Res, J Oral Maxillofac Surg, and Oral Maxillofac Implants, shows both flap and flapless procedures can yield high implant survival rates when clinicians follow evidence-based guidelines.
Clarify Aftercare and Healing Expectations
Different implant techniques can influence the healing process, soft tissue management, and postoperative expectations. Before your dental implant surgery, make sure you understand the following:
-
Healing time based on your surgical procedure
-
Expected postoperative discomfort
-
Soft food requirements during early recovery
-
Follow-up appointments for evaluating peri implant health
-
Signs of complications such as early implant failure or peri implant mucosa inflammation
Clear expectations help reduce anxiety and contribute to successful clinical and radiographic outcomes.
Choose a Team That Offers Both Options
Beware of one-size-fits-all implant techniques. A comprehensive implant treatment center should offer both flapless dental implant placement using a flapless technique and conventional flapped implant placement using a flap technique, tailoring the surgical approach to your anatomy, gingival biotype, alveolar ridge contours, crestal bone levels, peri implant soft tissues, and long-term implant function, especially for patients with missing teeth or varying degrees of bone loss.
At 4M Dental Implant Center, we use CBCT-driven planning, implantology principles, osseointegrated implants, evidence-based surgical procedures, and advanced digital workflows to ensure predictable results whether you need flapless dental implant surgery performed with a soft tissue punch, conventional implant placement using a mucoperiosteal flap, or immediate implant procedures with immediate functional loading followed by proper implant healing using a healing abutment, implant healing cap, or implant abutment as indicated.
Flapless or Flapped: Your Smile Deserves a Custom Strategy
The choice between flapless surgical techniques and traditional flap surgery isn’t about trends—it’s about trust, tailored care, and selecting the right surgical procedure for your anatomy. Our surgeons understand how factors such as crestal bone resorption, alveolar ridge anatomy, implant uncovering timing, implant survival, soft tissue healing, peri implant health, and implant function influence long-term outcomes, particularly in patients with compromised bone or soft tissue conditions.
From minimizing bone resorption and surgical trauma to maximizing esthetics and implant survival rates, every decision we make is rooted in clinical evidence and years of oral surgery experience, ensuring that bone loss is managed appropriately and each implant procedure supports long-term stability and function.
Schedule a Consultation and Know Your Options
Your dental implant journey starts with clarity. Whether flapless implant, flap surgery, or immediate implant placement is right for your case, we’ll explain the reasoning, show you the imaging, and guide you through each step.
Book your free 4M Smile Assessment today.
Get the answers, confidence, and care you deserve—so you can move forward with total peace of mind.