Tooth loss is a life-altering experience for anyone. But for cancer survivors, especially those treated for oral cancer, it often marks just one more obstacle in a long and difficult journey. The effects of radiation, chemotherapy, and ablative surgery can leave patients without the ability to chew, speak, or smile with confidence. Fortunately, advancements in implant dentistry and restorative dentistry now offer permanent, functional, and aesthetic solutions in the form of dental implants.
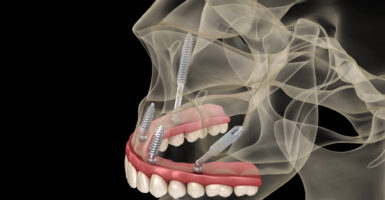
Whether you’ve experienced bone loss, loss of the mandible, or tissue damage following oral cancer reconstruction, today’s custom-made implants and full-arch dental implant systems provide life-changing results. At 4M Dental Implant Center, our team of implant dentists and surgeons can collaborate with medical professionals to create a personalized care and treatment plan designed to restore function and aesthetics, even after complex cancer treatment.
Let’s explore how dental implants can help oral cancer patients restore their smile, regain full oral function, and take back their quality of life through safe, modern implant surgery backed by advanced technology like CBCT scans, 3D CBCT imaging, and state-of-the-art dental materials.
How Oral Cancer and Its Treatment Cause Tooth Loss
Cancer affects every aspect of a person’s life, including their oral health. For those with head and neck cancer or oral cancer, tooth loss is a common consequence of both the disease and its treatments.
The Impact of Radiation and Chemotherapy
Radiation therapy, while crucial in treating neck and head cancers, often damages healthy tissues in the process.
When the jawbone and surrounding oral structures are exposed to radiation, patients may develop osteoradionecrosis, which is a condition where bone tissue dies due to a lack of blood supply. This severely compromises the structural foundation needed for teeth replacement and complicates denture fitting processes or implant surgery.
Similarly, chemotherapy (or chemo therapy as sometimes noted) can weaken the immune system and disrupt the mouth’s natural healing process. The result? A blow to dental health and increased risk of implant failure, infections, gum disease, and accelerated tooth decay, often culminating in total tooth loss.
Surgical Tooth Loss After Cancer Diagnosis
In some cases, patients may undergo ablative surgery to remove cancerous portions of the mandible or maxilla, leading to immediate loss of multiple teeth. These invasive surgical procedures are vital for stopping the cancer’s spread but leave behind a complex need for oral cancer reconstruction, not just for function, but for facial structure and identity.
Emotional and Functional Toll of Tooth Loss
The loss of teeth post-cancer diagnosis is more than cosmetic. It impairs chewing, speech, and erodes self-esteem. Patients often find themselves unable to eat nutritious foods, participate in social activities, or feel confident in their smile. This emotional impact can delay recovery, increase anxiety, and prolong the return to normal life, even after reaching remission.
The Role of Dental Implants in Restoring Health and Confidence
Losing teeth due to cancer can be devastating, but restoring your smile doesn’t have to be. Thanks to advancements in dental technology, dental implants have become a cornerstone of oral cancer reconstruction, offering both aesthetic and functional recovery for cancer survivors.
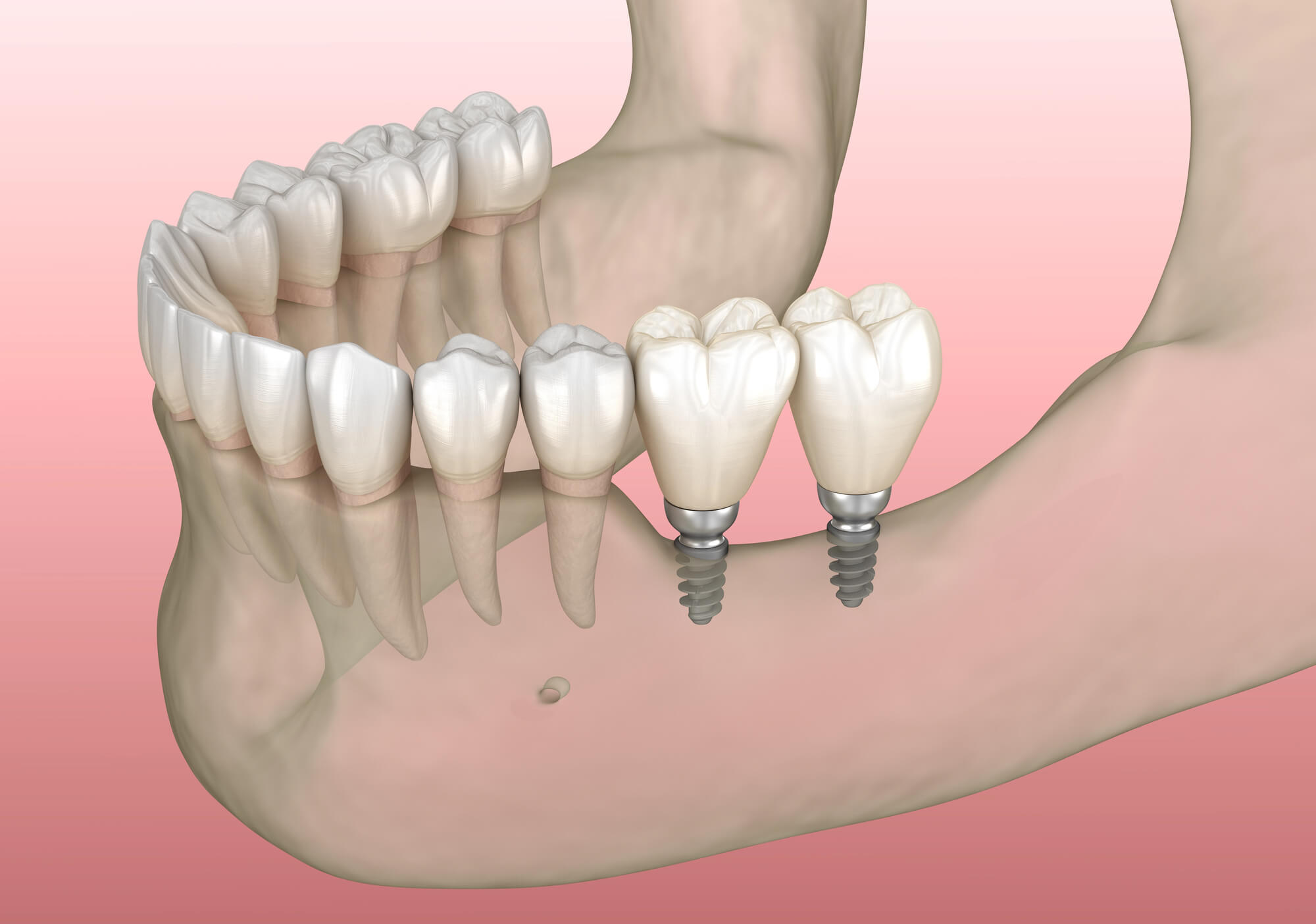
For example, 4M dental implants are not simply cosmetic: they are custom-designed, medically engineered dental prosthetics anchored directly into the jawbone.
They serve as artificial tooth roots, allowing for the placement of dental crowns, bridges, or implant dentures that look and function just like natural teeth.
Dental Implants vs. Dentures: A Transformational Upgrade
Traditional dentures often fall short in restoring bite power, stability, or confidence. They can slip, require adhesives, and do little to preserve the jawbone. Implant-supported solutions—like full-arch dental implants—eliminate these issues by fusing with the jawbone, preventing bone loss and offering superior comfort.
Cancer survivors often benefit from:
- Improved function for chewing and speaking
- Restored facial aesthetics and confidence
- Reduced bone resorption after ablative surgery or radiation
- Custom prosthetics tailored for fit and performance
- Permanent solutions with proper care and maintenance
At 4M Dental Implant Center, we use custom-made implants and high-grade dental materials to match each patient’s anatomy, goals, and medical history.
Cosmetic and Psychological Benefits
Tooth loss following cancer treatment often causes patients to feel like they’ve lost part of themselves. Dental implants can help restore not just a smile, but self-image, dignity, and the ability to connect socially. For many patients, regaining the ability to laugh without hesitation or eat without discomfort marks a powerful return to normalcy after cancer.
A Restorative Option for All Stages of Recovery
Whether you are newly in remission, midway through radiation treatment, or post-surgical procedures, dental implants offer staged options based on where you are in your recovery. Our implant dentists and prosthodontics team at 4M work closely with your oncologists and healthcare team to develop a safe, evidence-based dental implant treatment plan aligned with your medical and dental timelines.
Schedule Your Free Consultation
Are You a Candidate for Dental Implants After Cancer Treatment?
Determining your eligibility for implant surgery after a cancer diagnosis is complex, but far from impossible. While cancer treatments can complicate healing, advances in technology, surgical planning, and coordination between dental and medical providers make implants more accessible than ever, even for high-risk cases.
Key Factors That Affect Eligibility
Before starting any surgical process, your implant dentist will conduct a thorough medical history review, including:
- Type and location of cancer
- Whether radiation targeted the mandible or jawbone
- Presence of osteoradionecrosis
- Current health status and immune function
- Ongoing medications, such as bisphosphonates or immunosuppressants
A physical exam, intraoral inspection, and high-resolution 3D CBCT imaging are used to assess bone grafting needs, implant positioning, and the viability of your jaw structure.
Radiation Therapy and Jawbone Health
One of the biggest concerns for oral cancer patients is the impact of radiation on the jawbone. Radiation reduces blood flow, which can affect healing and the body’s ability to support implants. However, with proper planning, even patients with prior radiation treatment may qualify using:
- Advanced bone grafting techniques
- Staged surgical protocols
- Hyperbaric oxygen therapy (in select cases)
At 4M, we specialize in identifying safe paths forward for patients, including those who’ve undergone head and neck cancer therapies.
Customized Treatment Planning with a Multidisciplinary Team
Implant dentistry after cancer requires collaboration. That’s why 4M Dental Implant Center can work in tandem with oncologists, radiologists, and primary care providers to ensure every surgical and restorative decision supports your long-term health.
Our protocols integrate:
- Dental oncology risk assessments
- Interdisciplinary consults
- Pre-surgical planning aligned with your recovery window
Whether you need a single implant or a full-arch reconstruction, we customize every element of your treatment plan for safety, success, and full smile restoration.
Alternatives to Dental Implants After Cancer Tooth Loss
While dental implants are often the gold standard for restoring lost teeth, they may not be immediately feasible for all oral cancer survivors, especially those with extensive jawbone damage or delayed healing from radiation treatment or chemotherapy. Fortunately, there are alternatives and adjunctive procedures that may serve as temporary or permanent solutions depending on each patient’s needs.
Implant-Supported Dentures
For patients who have experienced partial bone loss but still have enough remaining jaw structure, implant-supported dentures offer a more stable alternative to traditional dentures. These solutions use two to four dental implants per arch to secure a removable denture, improving:
- Stability during eating and speaking
- Comfort compared to adhesive-based dentures
- Jawbone preservation through minimal stimulation
They’re especially ideal for patients awaiting full-arch dental implants in a staged recovery process.
Traditional Dentures and Bridges
When implant surgery is not recommended due to severe osteoradionecrosis, immune suppression, or ongoing cancer therapy, traditional dentures or dental bridges may serve as an interim solution. While they do not prevent further jawbone deterioration, these dental prosthetics can restore some function and aesthetics, helping patients eat, speak, and smile more comfortably.
- Bridges may be viable if adjacent teeth are healthy enough to support them
- Full or partial dentures can be custom-shaped for comfort and appearance
However, because these options lack root stimulation, they don’t support long-term bone health the way implants do.
Bone Grafting and Ridge Augmentation
In many cases, patients once considered “non-candidates” for dental implants become eligible after bone grafting or ridge augmentation. These surgical procedures rebuild jawbone volume lost through ablative surgery, radiation, or long-term denture wear.
At 4M Dental Implant Center, we use cutting-edge techniques such as:
- Platelet-rich plasma (PRP) and platelet-rich fibrin (PRF) to accelerate healing
- Ridge preservation following extraction
- Custom 3D-printed surgical guides for precise grafting
Our advanced planning systems, powered by CBCT imaging, allow us to determine grafting needs with millimeter precision, increasing treatment confidence and reducing risk.
How the 4M Dental Implant Center Approach Supports Cancer Survivors
More than just placing implants, restoring your smile after cancer is about rebuilding your confidence, health, and quality of life with safety, precision, and compassion. At 4M Dental Implant Center, we specialize in treating patients, enabling our team to identify risks early and ensure predictable outcomes.
Advanced Diagnostics and Technology
Before we begin treatment, our process includes a comprehensive medical history review and a diagnostic workup using the latest 3D CBCT imaging, modeling, surgical planning, and even virtual previews of results.
This level of precision enables our team to identify risks early and ensure predictable outcomes, even in medically complex cases.
Collaboration with Oncologists and Specialists
We don’t work in a vacuum. Our dentist and implant surgeons collaborate directly with your oncologists and healthcare providers to ensure all surgical and restorative decisions align with your cancer recovery plan.
Our team tailors every step of the treatment plan to your health, comfort, and future success.
Personalized Care Through Every Stage
At 4M, there is no one-size-fits-all solution. Whether you’re receiving a single dental implant, custom prosthetics, or a full-arch implant system, we deliver:
- Custom-made implants matched to your anatomy
- Flexible sedation options for anxiety-free surgery
- Post-op support kits for a smooth recovery process
- Access to same-day teeth replacement options when viable
Every element, from the denture fitting process to final dental crown placement, is centered on restoring your smile with maximum safety, comfort, and long-term function.

Healing, Recovery, and Implant Longevity After Cancer
The recovery process following implant surgery is critical to long-term success, especially for a cancer patient whose oral health, jaw, or inner cheek tissues may have been compromised by radiation therapy, chemotherapy, squamous cell cancer, neck cancer surgery, oral surgery, or ablative surgery that resulted in missing teeth or required tooth extraction. At 4M Dental Implant Center, our oral surgeon team creates healing protocols designed specifically for patients emerging from these complex medical and surgical journeys, including those transitioning from a denture to a more stable tooth replacement solution.
What to Expect During the Healing Phase
After your custom-made implant is placed during surgery, the surrounding jawbone begins a biological process called osseointegration, where bone fuses to the titanium post, creating a stable anchor for your dental prosthetic and long-term tooth replacement.
For patients without complicating factors, this process typically takes about 3–6 months. However, for individuals with a history of oral cancer, radiation therapy, or neck cancer surgery, healing timelines may be extended to protect oral health, preserve jaw integrity, and allow for careful monitoring following oral surgery or prior tooth extraction procedures.
You may receive:
-
Antibiotic support to prevent infection following surgery
-
PRF or PRP regenerative therapies to enhance healing of the jaw and inner cheek tissues
-
Nutritional and hygiene guidelines tailored to oral health recovery and denture-to-implant transitions
Our team closely monitors your dental implant sites with digital imaging and routine check-ins to ensure osseointegration progresses properly and that healing remains stable for each cancer patient.
Factors That Influence Recovery
Some patients require lifestyle adjustments or pre-implant interventions to optimize healing and implant longevity, particularly those who have:
-
Used tobacco or alcohol, which can impair blood flow to the jaw
-
Experienced osteoradionecrosis after radiation therapy
-
Taken medications such as bisphosphonates or corticosteroids following cancer treatment
Additionally, patients must maintain excellent home care throughout recovery, including gentle brushing, antimicrobial rinses, and avoiding pressure on the surgical site after oral surgery or tooth extraction. Proper care supports long-term oral health and improves outcomes for those replacing missing teeth after cancer treatment.
Our dental office provides continuous education, monitoring, and personalized support throughout the healing process to help every patient achieve a successful, durable outcome following surgery and implant placement.
Longevity of Dental Implants After Cancer
With proper care and placement by experienced implant dentists, dental implants have a success rate exceeding 95%, even for patients with past cancer treatment. At 4M, our custom protocols and high-precision surgical guides help reduce risks and ensure your teeth replacement lasts for decades.
We support our patients with:
- Post-op maintenance plans (4M Smile Wellness™)
- Regular hygiene checkups and implant monitoring
- Education on preserving gum and bone health long-term
Realistic Expectations: Risks, Success Rates, and Innovations
As with any surgical procedure, it’s essential to understand both the benefits and the potential risks of getting dental implants after oral cancer. At 4M Dental Implant Center, we believe in transparency, education, and evidence-backed decisions so patients feel empowered throughout their care journey.
Understanding Potential Risks
Patients who have undergone radiation treatment, chemotherapy, or ablative surgery may face higher risk factors, such as:
- Delayed healing or osseointegration issues
- Increased risk of implant failure due to poor vascularization
- Complications from previous infections or bone loss
That said, these risks can be mitigated with proper screening, CBCT scans, careful surgical technique, and collaboration with your oncology team.
We also review:
- Pre-existing conditions (e.g., diabetes, autoimmune disorders)
- Current medications
- Any history of failed prosthetic devices
Success Rates Among Cancer Survivors
Thanks to advances in restorative dentistry, most oral cancer survivors can achieve long-lasting results from custom dental implants, with success rates approaching those of patients without prior cancer diagnoses.
Our experience with complex cases enables us to adapt and succeed where more generalized practices may hesitate.
Innovations That Make a Difference
4M Dental Implant Center remains at the forefront of technology. From our denture fitting process to our same-day implant denture systems, we implement cutting-edge tools to maximize comfort, safety, and outcomes.
These tools help us reduce surgery times, eliminate guesswork, and deliver personalized care with exceptional predictability, particularly important for cancer survivors seeking comprehensive oral health restoration.
Schedule Your Free Consultation
When to Consider Dental Implants After Cancer Treatment
Knowing the right time to pursue dental implants after cancer treatment is just as important as the dental implant procedure itself. For patients recovering from oral cancer, head and neck cancer, or related malignancies, dental implant treatment must be carefully timed and medically coordinated. Every survivor follows a different healing path, and implant placement should only proceed once oral health, bone density, and soft tissues have stabilized.
Dental implants oral cancer patients receive require a multidisciplinary approach that accounts for surgical treatment history, cancer development risk, and long-term oral rehabilitation goals. Collaboration between your oncology team, oral implantology specialists, and implant dentists ensures a safe, evidence-based decision.
Recommended Timeline After Radiation or Chemotherapy
In most cases, implant treatment is delayed until the body has had adequate time to recover from:
Radiation therapy to the oral cavity, jaw bone, or head and neck region, typically 6–12 months post-treatment, depending on dose and field exposure
Chemotherapy or immunosuppressive therapy, as directed by your oncologist and guided by a detailed risk patient report
Resective surgery or ablative procedures that may have altered alveolar bone, facial structure, or peri implant tissues
Patients treated for oral squamous cell carcinoma, squamous cell carcinoma of the oral mucosa, or invasive carcinoma of the neck region often require extended monitoring due to known risk factors such as chronic inflammation, tobacco smoking, heavy alcohol consumption, viral infections, and genetic predisposition. These factors may increase the risk of peri implant inflammation or peri implant bone loss if implants are placed too early.
Your dental office works closely with your oncology providers to monitor healing, evaluate growth factors and bone regeneration, and determine when dental osseointegrated implants can be placed safely.
Signs You’re Ready for Dental Implants
You may be ready to consider dental implant therapy if:
Your cancer is in remission, with no evidence of developing cancer or malignant lesions on follow-up imaging
Your oral health has stabilized, with no active oral lichen planus, poor oral hygiene, or untreated periodontal disease
A comprehensive review of risk factors, including alcohol consumption, tobacco use, and irritant factors, shows manageable potential risks
You have adequate jaw bone volume, alveolar bone support, and bone density, or you are a candidate for grafting prior to replacing missing teeth
Advanced CBCT imaging, clinical evaluation, and differential diagnosis help confirm that implant placement will not interfere with early detection of squamous cell carcinoma appearing or unusual recurrence patterns. Special attention is given to peri implant tissues, oral mucosa, and soft tissues to avoid masking clinical features of oral carcinoma.
Preparing for Your Consultation
Your first step is a consultation at one of our 4M Dental Implant Center locations, where we will:
Conduct a complete medical and dental history review, including prior cancer treatment, surgical treatment records, and inclusion criteria for implant therapy
Perform digital scans and imaging, including 3D CBCT, to evaluate bone density, alveolar bone, and anatomical structures of the oral cavity and head and neck
Evaluate existing prosthetics or missing teeth, including considerations for edentulous patients and complex reconstructions
Develop a customized treatment plan outlining implant placement options such as osseointegrated dental implants, symphyseal dental implants, or alternative solutions like a mandibular staple implant when indicated
We also assess oral hygiene habits, periodontal ligament health, peri implant mucositis risk, and long-term oral function to ensure the medical procedure is both successful and sustainable.
Empowering Your Smile After Cancer with 4M Dental Implant Center
Your cancer journey reflects resilience. Restoring oral function and confidence through dental implants should reflect that same strength, using solutions grounded in clinical experience and supported by properly cited research from sources such as J Oral Maxillofac Surg and Clin Implant Dent Relat Res, including systematic review findings and open access article distributed data where appropriate.
At 4M Dental Implant Center, we specialize in dental implants for medically complex patients, including those treated for oral carcinoma, squamous carcinoma, breast metastasis to the jaw, or unusual case report scenarios involving rapid evolution or unusual occurrence of exophytic lesion growth.
Our team understands the balance between oral rehabilitation and vigilance. We design implant therapy that supports replacing missing teeth while preserving visibility for early detection, protecting peri implant tissues, and minimizing increased risk related to several risk factors.
With advanced oral implantology techniques, careful management of peri implant inflammation, and long-term follow-up, we help patients regain oral function, stability, and confidence—without compromising safety.
Schedule your consultation today and take the next step toward restoring your smile with osseointegrated implants, precision planning, and hope—guided by expertise, compassion, and evidence-based care.